Practice Management Tips
April 2024
Successful Practice Transitions
Are you considering a practice merger, sale or acquisition? Taking time to define your values, needs, wants and overall objectives prior to initiating the process will have a direct impact on your satisfaction post-event. Assembling a team of experts – accountant, lawyer, appraiser – is a must to help the process go smoothly.
For any change:
Plan as far in advance as possible and have a timeline for specific tasks. Many physicians underestimate the time needed; ideally you’ll have 6-12 months but some transitions will require more or less.
Make sure you understand the impact on
- Your administrative and clinical teams – some turnover is normal, and having a plan to address this ahead of time will be helpful.
- Patient care/the way you practice – if you’re giving up control of some aspects of the practice, be very clear what you can and cannot compromise on.
- Technology – if you’re merging with another group, which EHR/appointment reminder system/practice management system will be used, and will there need to be training?
- Partnerships – how are proceeds from a sale being divided among partners/employee physicians/key team members?
Want to learn more? Make plans to attend the 2024 Practice Management Workshop July 12-14 in Denver and attend the session on Practice Mergers, Acquisitions and Partnerships. Or visit the AAAAI website and view our resources for buying, selling and closing a practice.
March 2024
Collecting deductibles and co-insurance at time of service
Does your practice have a policy to collect deductible and coinsurance payments at the time of service but struggle to collect them routinely? Try one (or more) of these approaches suggested during a recent discussion on the AAAAI Practice Manager Network:
If staff are uncomfortable asking for payments:
• Develop a script and coach them on how to deliver the request confidently
• Practice role playing during a staff meeting to increase confidence
• Encourage your front desk staff to say “HOW would you like to pay your balance today?” instead of “WOULD you like to take care of your balance today?” This sends a clear message that payment is expected and provides options for payment.
• Share patient balance collections on a daily or weekly basis with the entire front desk team. This may result in some friendly team competitiveness and higher collections overall.
Put these protocols in place before the patient arrives:
• Message the patient the day prior to the appointment with their amount due so they come to the office prepared to make a payment
• Create a credit card on file policy for your office so that you are able to collect payment automatically within a certain time frame, such as 30 days after a statement has been sent
• If you’re able, utilize your immunotherapy system technology to block checking in for shots if there is a balance due. The front desk team can approve the shot after payment is received.
The AAAAI Practice Manager Network is a private Facebook group open only to staff working with AAAAI member allergists. Want your manager and/or other staff members to have access to this valuable resource? Send an email to practicemanagement@aaaai.org.
Grow your network and get more practice management knowledge at the 2024 Practice Management Workshop July 12-14 in Denver, CO. If you can’t attend yourself, send one (or more) of your team members.
February 2024
Independent Contractor Rule
If your practice works with an independent contractor, you need to make sure you are complying with the new Department of Labor (DOL) Independent Contractor Rule that takes effect March 11, 2024. Practices that misclassify workers as independent contractors when they should be considered employees could face penalties.
The new rule considers several factors when determining if a worker is an employee or an independent contractor:
• Opportunity for loss or profit depending on managerial skill
• Investments by the worker and the potential employer
• Degree of permanence of the work relationship
• Nature and degree of control
• Extent to which the work performed is an integral part of the potential employer’s business
• Skill and initiative
This article on the DOL website provides a good overview of the rule and how determinations are made for each factor.
If you are attending the AAAAI Annual Meeting in Washington, DC, visit the Practice Management Hub and talk with our legislative and regulatory experts.
January 2024
Handling Disruptive Patient Behavior
While most patients are a pleasure, every practice has had the unfortunate experience of having to deal with unreasonable, disruptive and even dangerous persons. Here are some tips to minimize the negative effects on staff, clinicians and other patients:
Set expectations
Develop a patient’s rights and responsibilities document that clearly outlines the type of behavior expected by the practice and post it in a highly visible area. Include information on:
• Respect for physicians and staff
• Protocols for refilling medications, appointment cancellations, etc.
• Behaviors with a zero tolerance policy, including physical and verbal abuse
When an incident occurs, document this in the patient record in case termination becomes necessary.
Prepare your team
Develop a written policy for handling disruptive patient behavior and train staff regularly. Prepare for potential encounters by role playing and have team members share their experiences with defusing difficult situations. Discuss as a group how various situations can be effectively resolved.
Make plans now to attend the 2024 Practice Management Workshop July 12-14 in Denver, CO and attend the session on Managing the Wellbeing of the Entire Practice Team: Wellness, Burnout and Dissatisfaction Among Patients, Staff and Physicians.
For more information, view this presentation from the Connecticut Academy of Family Physicians and read this article from Physicians Practice.
December 2023
Penicillin Allergy Testing
While 10% of the United States population believes they are allergic to penicillin, allergist / immunologists know that the vast majority are not. Identifying individuals in your community who believe they are allergic and offering testing to potentially de-label their penicillin allergy can result in:
• Faster, safer and more effective treatments for patients
• Significant cost savings for patients, physicians and health systems
• Reduced levels of antibiotic resistance
Visit the AAAAI Penicillin Allergy Center for practical resources to use with your patients and educational materials for you and your practice team. JACI: In Practice also has a curated collection of updated drug allergy resources.
November 2023
Negotiating Managed Care Contracts
Are you one of the many allergy practices experiencing declining payer reimbursements? Strengthen your position during your next contract renewal term by:
Knowing your contracts. Create a contract summary form that includes the fee schedule, effective dates, contract point outliers, etc. for each payer. Be clear on what each payer’s reimbursement level is and don’t charge less than a payer will reimburse.
Being prepared with the data. Gather patient quality data and make the case for your practice. What needs are you meeting/what treatments are you offering that others in the marketplace are not? Calculate the break-even point for your practice ahead of time.
Negotiating like a pro. Treat negotiation like a process, not an event. Your first plan generally won’t survive the first round; be prepared to adapt, adjust and overcome. Set goals for your negotiation. Reimbursement rates are essential, but contract language can be just as important. Be clear on your walk away points.
Visit the AAAAI website for more contract negotiation strategies and make plans now to attend the 2024 Practice Management Workshop July 12-14 in Denver, CO. You won’t want to miss our session “Negotiating Managed Care Contracts – Secrets from a Former Managed Care Executive.”
October 2023
Prepare Your Practice for USP 797: Practical Tools for Your Practice
The AAAAI Compounding Corner has practical tools your practice can use to ensure you’re in compliance with the new USP 797 guidelines taking effect November 1. In this month’s guest editorial, Mohamed Yassin, MD, FAAAAI, shares samples used in his practice, including an AIT compounding log and standard operating procedures for the compounding process.
Review these steps to prepare and contact practicemanagement@aaaai.org with your USP 797 questions.
September 2023
Prepare Your Practice for USP 797: New Allergen Extract Label Requirements
The new USP 797 guidelines taking effect November 1 include revised allergen extract labeling requirements, and we have heard from practices that payers are already expecting to see the new label formats and are denying payment.
The label of each vial of an allergenic extract prescription set must display the following prominently and understandably:
• Patient name
• Type and fractional dilution of each vial, with a corresponding vial number
• Beyond use date (BUD)
• Storage conditions
View an example of a compliant vial label in the Compounding Corner.
Listen to session “Preparing Allergen Immunotherapy Extracts” presented at the 2023 AAAAI Practice Management Workshop to get a complete overview of USP 797 requirements and tips on how to prepare your practice. This recording is available to AAAAI members at no charge as a member benefit.
Questions related to USP 797 guidelines can be sent to practicemanagement@aaaai.org.
August 2023
Is Work From Home Right for Your Practice?
Prior to the COVID-19 pandemic, remote working options for medical practices were minimal. Now, more than half of medical practices report that up to one quarter of their team works remotely, and employees are reluctant to return to the clinic full time.
Medical practices offering flexible work schedules have seen increases in productivity, revenue, and employee morale and retention. Even better, the costs to pivot to a remote or hybrid schedule are small, with most practices reporting an investment of $5,000 or less.
Benefits to practices with remote and hybrid working schedules include:
• Broadening the pool of candidates for clinical and administrative team members
• Increasing job satisfaction/improving employee morale
• Reducing costs through smaller office square footage needs
It’s important to remember that a full review and assessment of operations with all team members (practice managers, clinical team, technical support) is a critical first step in ensuring the arrangements will work for your practice.
Learn more about steps your practice can take to attract and retain a high functioning team by listening to the recordings from the 2023 Practice Management Workshop.
July 2023
Prepare Your Practice for USP 797: Staff Training and Competency Requirements
The new USP 797 guidelines taking effect November 1 include requirements for staff training and competency, and the AAAAI has the resources you need to ensure your compounding team is prepared ahead of the deadline.
Allergen extract preparation quiz
All compounding personnel are required demonstrate knowledge and competency in allergen immunotherapy extract preparation and sterile compounding procedures by passing written or electronic testing. The AAAAI quiz is one option for practice staff to demonstrate this competency (but not the only option).
Subcutaneous Allergen Immunotherapy Extract Preparation for Aeroallergens and Venom
This chapter from the Practice Management Resource Guide has been updated to reflect the new USP 797 guidelines and is an excellent resource for your team.
The AAAAI Compounding Corner has illustrated handouts for the following competencies:
• Gloved fingertip and thumb sampling – team members must successfully complete gloved fingertip and thumb sampling on both hands no fewer than 3 separate times prior to compounding. After initial competency is demonstrated, follow-up testing is required annually.
• Garbing and hand hygiene
• Media fill testing – compounding team members must have their sterile technique evaluated at least every 12 months by successful completion of a media fill test.
All team member training and competency activities must be documented. Individuals who fail competency evaluations must successfully pass reevaluations in the deficient area(s) before resuming compounding duties. A designated person within the practice must identify the cause of failure and determine appropriate retraining requirements, and all training compliance should be logged. The AAAAI has provided a sample log in the Compounding Corner.
Questions related to USP 797 guidelines can be sent to practicemanagement@aaaai.org.
June 2023
Prepare Your Practice for USP 797: Compounding Facility Requirements
With just under five months until the USP 797 guidelines go into effect, now is the time for your practice to review your space and protocols and plan for any changes that need to be made before November 1.
Allergy practices have two options for their allergen extract compounding space: a dedicated allergen extract compounding area (AECA) or an ISO Class 5 PEC hood. Both of these options require the following:
• Must be located away from unsealed windows, doors that connect outdoors, and traffic flow
• May not be located adjacent to environmental control challenges (restrooms, warehouses, food prep areas)
• Must be at least 1 meter away from sinks
• Impact of activities around or adjacent to PEC or AECA must be considered
If your practice is planning to use an AECA, you may need time to update your current space or create a new area. Review the facility requirements here (link to updated document when available).
Visit the Compounding Corner, your central hub for everything you need to make sure you’re in compliance by November 1.
May 2023
Mobile Health Technologies (mHealth) Can Increase Patient Engagement/Adherence and Improve Outcomes
The availability and use of remote monitoring devices and mobile health (mHealth) applications (apps) has expanded exponentially in the past three years. Today, 95% of US adults aged 18-49 own a smartphone as do 61% of adults over age 65.
mHealth apps are widely available in a variety of formats (smartphones, tablets, computers, wearable technology) and are viewed positively by both patients and physicians. Apps offer symptom diaries, educational content, medication reminders, patient self-tracking dashboards, goal setting/behavior change techniques and more. They can also provide patient reported outcomes (PROs) that encourage shared decision-making and collect data outside the traditional clinic setting.
mHealth interventions have been shown to favorably impact clinical, economic and process outcomes and have been linked to:
• Improvements in patient knowledge and medication adherence
• Improvements in asthma control and quality of life
• Fewer unscheduled office visits
Learn more about incorporating remote monitoring devices and mHealth apps into your practice by attending the “Remote Patient Monitoring: Tech and Tools for Success” session at the 2023 AAAAI Practice Management Workshop (July 28-30 in Minneapolis, MN).
Read more here:
mHealth and Allergy/Immunology (AAAAI article)
Drive patient retention with remote patient monitoring (Physicians Practice article)
Remote patient monitoring: building a new outpatient revenue stream (MGMA article)
April 2023
Some telemedicine provision flexibilities expire with the Coronavirus Public Health Emergency (PHE)
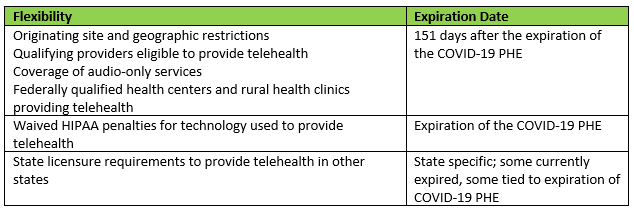
The COVID-19 public health emergency (PHE) ends on May 11 and when it does, many flexibilities related to the provision of telehealth services will also end. While some provisions will remain in place temporarily, others will end immediately.
For the telehealth flexibilities ending on May 11, the Office of Civil Rights (OCR) is providing a 90-day transition period during which they will not impose penalties on non-conforming physician practice to allow time for offices to meet the requirements (ends August 9, 2023).
The AAAAI continues to support legislation designed to make many of the PHE flexibilities and waivers permanent. You can read more about our efforts here.
A comprehensive summary of COVID-19 related flexibilities can be found here.
March 2023
Allergy Practice Staffing Ratios
There is no one-size fits all staffing ratio for an allergy practice; team size and staff composition varies widely based on a number of factors. Here are some ways you can determine the best team for your practice:
• Consider the level of services your practice provides – clinical care, allergy injections, biologics administration, and procedures all contribute to your staffing needs.
• Conduct a careful review of your current staffing levels, taking care to identify any redundancies currently in place. Are your team members operating at the top of their scope of practice?
• Cross-training staff can help alleviate short term issues due to illness, vacations, etc.
Speakers at the 2022 Practice Management Workshop provided a sample staffing ratio for a mostly full allergy practice with one physician:
• Clinic nurse
• Mixing and injection nurse
• Procedure nurse
• Biologics coordinator
• Front desk/first impression specialist (often cross-trained)
• Check-out/financial counseling specialist
• Coder/biller
• Accounts receivable specialist
Learn more by listening to the PMW recording Strategies for Hiring and Developing an Allergy/Immunology Team.
February 2023
Practice Changes: Moving, adding or consolidating locations
A recent STAT poll from the Medical Group Management Association (MGMA) showed 53% of physician practices are planning to add or relocate a practice facility in the next two years. If you’re considering something similar, planning is critical. Here’s how to map out a successful transition:
1. Give yourself enough time – Moves are complicated. Give yourself at least 6-12 months to work through all of the steps. Expect the unexpected and have a plan to change course when necessary.
2. Verify dates with key vendors/suppliers well in advance – Check in with utilities, your phone service provider, waste management, water delivery service, etc. to ensure everyone is on the same schedule.
3. Notify insurance and credential providers of the move – As soon as you have a date set, reach out to your insurance providers. You’ll want to updated your NPI, DEA and license with the new address, which can take more than 3 months.
4. Transition patient care seamlessly – Post signs in the office, call patients to remind them about the move, include information on billing statements.
For more information, listen to the 2022 Practice Management Workshop session recording "Practice Changes: Buying, Selling, Moving."
January 2023
Practice Changes: Selling Your Practice
Are you considering selling your practice? Preparation and a clear sense of your goal for the sale is crucial. Take these steps to ensure your success:
1. Clearly define the "why". Are you looking to reduce administrative burdens, increase your competitive advantage, or find a better balance between your personal and professional life? Make sure your sale partner will allow you to accomplish those goals.
2. Know what you are (and aren't) willing to change. Will there be new rules that affect your ability to care for your patients the way you see fit? How will the sale affect your staff, particularly the key members of your team?
3. Know the value and selling points of your practice. Do you offer sought after treatments, have a healthy financial bottom line and a strong management team? Leverage your practice's strengths to your advantage.
4. Invest in high quality consultants. Having a competent legal and/or management consultant to guide you through the negotiation is money well spent.
For more information, listen to the 2022 AAAAI Practice Management Workshop session recording, "Practice Changes: Buying, Selling, Moving."
December 2022
Expand and Grow Your Practice in 2023
Is your allergy practice looking to expand in 2023?
At the 2022 Practice Management Workshop, faculty had several recommendations for new services that increase value and patient satisfaction:
• Establish or expand penicillin allergy testing. While 10% of the U.S. population is labeled as penicillin allergic, we know that 90% of those individuals are not truly allergic when fully evaluated. Access the myriad resources available in the Penicillin Allergy Center.
• Add infusion services such as biologics, immunoglobulin, hydration therapies and other medications (antibiotics, corticosteroids).
• Maximize procedures. Endoscopy, fractional exhaled nitric oxide (FeNO), patch testing, rush/cluster immunotherapy and others are discussed by program faculty as ways to potentially add value to your practice.
Learn more by listening to the 2022 Practice Management Workshop recordings “Enhancing Practice Revenue with Additional Services.” Register for virtual access here.
November 2022
Tracking COVID-19 Public Health Emergency Flexibilities and Waivers
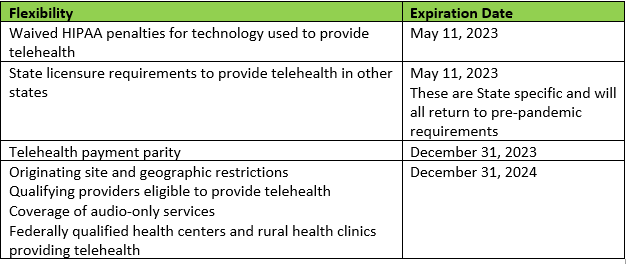
The COVID-19 public health emergency (PHE) was established in December 2020 and is currently in effect through January 11, 2023. Under the PHE, federal agencies have the ability to waive certain requirements to support the continued access to critical healthcare services. Those most relevant to allergy/immunology are related to telehealth. Here is a summary of the current flexibilities and waivers and their expected expiration date:
The AAAAI continues to support legislation designed to make many of the PHE flexibilities and waivers permanent. You can read more about our efforts here.
A comprehensive summary of flexibilities related to COVID-19 can be found here.
October 2022
Keeping in Compliance With Information Blocking Rules
Information blocking requirements have been in effect since April 2021, but the requirements applied to a narrow set of electronic health information (EHI) to allow practices time to develop and implement procedures to comply with the new law. As of October 6, the requirements apply to the entire EHI, including items such as medical images, assessment and plan of treatment, and clinical notes.
Here are some steps your practice can take to ensure you are in compliance:
• Designate someone within the practice to be the point person for information blocking issues.
• Review all existing policies and procedures for receiving, processing and responding to requests to access, exchange or use EHI, and revise them as necessary.
• Coordinate with your health IT vendors to ensure you are able to support patient EHI access requests.
• Establish a process for exceptions.
• Document all policies, procedures and actions developed by your practice to comply with information blocking regulations.
• Train your staff.
Our advocacy partner, Hart Health Strategies, has developed a briefing document to help members make sense of the new regulations. A primer on information blocking and other helpful resources is available here.
September 2022
Keep Your Practice on Track With a Strategic Plan
The most successful allergy practices have a clear vision of what they want to accomplish and a strategy to achieve that vision. Having a strategic plan will help you create a clear vision for future success and growth, identify short and medium term priorities and get buy-in from your team. At the 2022 AAAAI Practice Management Workshop, speakers provided these tips for getting started:
• Develop a vision and determine priorities, procedures and strategies.
• Understand your current financial picture and how that positions your practice for potential growth.
• Aim for a 12-month plan. Longer range planning can be difficult in a shifting healthcare landscape.
• Don’t put your strategic plan on the shelf. The best plans are ones that you regularly review and refine.
For more ideas, listen to the session “Strategic Planning for an Allergy/Immunology Practice” presented at the 2022 Practice Management Workshop.
August 2022
Mastering the Art of Contract Negotiation
Anyone can be a successful negotiator – it just takes preparation, clear understanding of your “must haves” and a willingness to compromise to get to a win-win situation.
Speakers at last month’s AAAAI Practice Management Workshop shared their tips for success:
Consider the ABCs
• Alternatives – identify, then refine them
• Beliefs – identify the critical uncertainties, quantify when able
• Consequences – identify them
Know What You Want
• Identify your “must haves” – what are you not willing to compromise on?
• Identify your “nice to haves” – where can you compromise to get to a win-win?
• Get advice from trusted others, but remain clear about your purpose (avoid confirmation bias)
• Research – what is possible and appropriate, what are the relevant standards/comparisons?
Negotiation Strategies
• Know your BATNA (best alternative to no agreement) and try to guess the other’s BATNA.
• Identify the ZOPA (zone of possible agreement).
• Know the difference between ideal and BATNA, and recognize the joint gains that come from compromise.
• Practice ahead of the meeting to build confidence.
• Recognize your value and what special skills and experience you bring to the table.
Listen to “The Ins and Outs of Contract Negotiation” by purchasing the 2022 Practice Management Workshop recordings.
July 2022
Minimizing Practice Errors – Incident Reporting Pearls
Mistakes are inevitable in medicine. Every allergy practice should have a system in place to collect healthcare event data with the goal of improving patient safety and care quality.
Incident reports should:
• Include the facts (no editorializing or subjective interpretations of the event)
• Include every individual involved (not to place blame, only to gather the most complete set of facts possible)
• Be completed as soon as possible after the event
Post-event, the practice should conduct a root cause analysis to identify which system(s) contributed to the error and what change(s) should be made to add a new layer of safety.
Learn more by listening to the 2022 Practice Management Workshop recording “When Mistakes Aren’t Mistakes: Turning a Negative into a Positive.” Register for virtual access here.
June 2022
Is Your Practice Prepared for the New USP-797 Guidelines?
The USP-797 standards for sterile compounding are likely to go into effect in early 2023 after a series of delays. Take some time now to review the new guidelines and ensure your practice is prepared. The Compounding Corner provides a wealth of resources for you and your staff, including personnel training procedures, an educational module, and summary documents for facility requirements.
Get the most up-to-date information and practical guidance at the AAAAI Practice Management Workshop, July 22-24 in Washington, DC. Sunday’s plenary session is dedicated to “Mixing Allergy Serums, Safe Administration, and Compliance with USP 797 Guidelines.”
May 2022
Delivering Patient-Centered Allergy Care
Your patients come to you for high quality, compassionate allergy care. They recommend your practice to friends and family based on a positive patient experience that includes much more than their allergy care. Here are ways you can ensure the best patient experience:
• Employ a patient-oriented team. The attitude of your staff can make or break your practice. Ensure a positive team by fostering a culture of cooperation, coaching team members and leading by example. Empower your staff to serve the patient.
• Ensure billing transparency. Make it easy for patients to know how much their treatment will cost, what their share is after insurance, and how to pay balances.
• Maintain a pleasant office environment. The waiting room should be neat and clean, furnishings up to date (not shabby or damaged), and office space easy to navigate with access points well-marked.
• Simplify your patient portal. Patients should be easily able to log in and view messages, test results and billing statements.
For more tips on optimizing patient experience, register for the 2022 AAAAI Practice Management Workshop, July 22-24 in Washington, DC, and attend the session “Building a Successful, Patient-Centered Allergy Practice.”
April 2022
Performing Patch Testing
Starting or expanding patch testing in your practice can be an excellent way to boost practice income and patient satisfaction. Here are some tips on how to identify appropriate patients and get started presented by Luz Fonacier, MD, FAAAAI, at the 2022 AAAAI Annual Meeting:
• Patch testing is the only way to accurately diagnose allergic contact dermatitis.
• Good candidates for patch testing include patients with:
o Chronic, itchy, eczematous dermatitis
o Persistent or recalcitrant dermatitis
o Atopic dermatitis who fail to improve
o Systemic contact dermatitis
• You can use commercially available screening series and personal patient products.
• Code visits appropriately for maximum reimbursement (see presentation slides linked below for details).
• Make sure you are aware of each individual insurer’s requirements and limits.
View Dr. Fonacier’s presentation slides here.
For more ideas on how to expand your practice, register for the 2022 AAAAI Practice Management Workshop, scheduled for July 22-24 in Washington, DC.
March 2022
Physician Onboarding Strategies
You’ve just found the perfect physician to add to your team. Ensure their success and protect your investment by taking time to fully integrate them into your practice. According to a recent New England Journal of Medicine article, the cost of hiring a physician who doesn’t fit and then leaves can add up to more than $1 million when you consider the expense of recruiting, onboarding, and filling the vacancy.
Here are some ways to keep everyone happy and productive:
• Automate your onboarding process. Take the time to develop a single plan you can use with all new hires. Everyone starts with the same expectations, the process is the same for all and you ensure that no key pieces of information are overlooked.
• Engage all of your physicians on every level. Send a welcome letter or gift box prior to the first day, set up a team lunch the first week, and assign a mentor to help the new physician navigate the practice.
• Be realistic about ramp-up time. New physicians need time to get acclimated to the practice’s workflows, systems and protocols, and building a new patient base can take some time. Allow 6-8 months (or more) for the new hire to get up to speed.
Visit the AAAAI website for more great hiring/recruitment tips and don’t forget to make plans to attend the 2022 Practice Management Workshop, July 22-24in Washington, DC.
February 2022
Keep Your Practice on the Right Track with Simple Benchmarks
Every allergy practice needs to have a strategic plan and financial benchmarks, and they don’t need to be sophisticated to be effective.
For small practices, develop a simple list of goals to accomplish during a specific time period and track revenue and expenses month to month to spot trends. Larger groups may have more advanced ways to track key performance indicators. Not sure what to track? Here are some resources to get you started:
• Benchmarking Basics: Key Indicators for a Healthy Practice (2018 AAAAI Practice Management Workshop presentation)
• Using Simple Bookkeeping Principles and Reports to Analyze Allergy Practice Performance (AAAAI Practice Management Resource Guide, Chapter 12)
• Financial Management and Fraud Prevention for the Allergist (2021 AAAAI Virtual Practice Management Workshop recording)
January 2022
Handling Staffing Challenges
The ongoing COVID-19 pandemic continues to create clinical and administrative staffing headaches for allergy practices. According to the Medical Group Management Association (MGMA):
• 33% of practices have had a physician leave unexpectedly in the last year.
• 73% rank staffing as their biggest challenge heading into 2022.
• 88% are having a difficult time recruiting medical assistants (MAs).
If your practice is experiencing the same issues, here are some ways to meet the challenges head on:
• Consider hiring CNAs to work under your LPNs and RNs—instead of MAs—and rename the position “Clinical Assistant”.
• Offer flexibility whenever possible—in scheduling, compensation, and benefits—to attract and retain top talent in this competitive job market.
• Ensure your current team members are working at the top of their licensure and ability.
• Consider candidates with customer service and/or call center experience for front-end duties and rename the position “Patient Engagement Specialist”.
For more tips on how to handle clinical and administrative staffing challenges, listen to the 2021 AAAAI Virtual Practice Management Workshop recordings, and read this MGMA insight article.
December 2021
Wealth Management Strategies For You and Your Practice
The end of the year is a good time to take a fresh look at your financial goals for the next year and change course as needed. Here are some tips presented during the 2021 AAAAI Virtual Practice Management Workshop:
• Live below your means. Physicians start their first job relatively late in life and may have little or no financial experience and a significant debt load. Aim to save at least 15% of your gross income each month.
• Invest early and often. Diversify your investments to include an appropriate allocation of stocks and bonds, and make sure you are investing appropriately for your age and risk tolerance.
• Maximize your tax efficiency. Take advantage of tax-deferred plans like 401(k), 403(b), IRAs, 529s and HSA accounts. These allow your investments to grow tax-free.
You can purchase access to “Wealth Management Strategies for the Practicing Allergist” and all 21 other sessions presented during this summer’s AAAAI Virtual Practice Management Workshop here. We also look forward to welcoming you back to an in-person 2022 AAAAI Practice Management Workshop, scheduled for July 22-24 in Washington, DC.
November 2021
It’s Never Too Early for Physician Succession Planning
Six months before you want to retire is the wrong time to think about turning over the reins to your practice to a successor. Ideally, your succession plan is something that has been developed over time that will serve as a tool to help ensure your practice continues to thrive after your departure. Even if retirement is in the distant future, it’s never too early to start planning, because:
• Timing issues can be beyond your control. A health scare, a pandemic, or other external forces can have immediate impact on your practice.
• Grooming the right successor can take time and may require a lengthy apprenticeship period.
• Your succession plan is never set in stone, and can change course to accommodate your changing needs.
Read more about succession planning in this article from Physicians Practice.
October 2021
HIPAA and COVID-19 Vaccine Status
Does asking for a practice team member’s or patient’s COVID-19 vaccine status violate HIPAA regulations? Not according to the recently issued guidance from the Office of Civil Rights, which notes that the HIPAA privacy rule does not prohibit:
• Businesses or individuals from asking whether their customers or clients have received a COVID-19 vaccine.
• Customers or clients of a business from disclosing whether they have received a COVID-19 vaccine.
• An employer from requiring a workforce member to disclose whether they have received a COVID-19 vaccine to the employer, clients, or other parties.
• A covered entity or business associate from requiring its workforce members to disclose to their employers or other parties whether the workforce members have received a COVID-19 vaccine.
Read more about HIPAA and COVID-19 vaccine status in this article from the HIPAA Journal and this overview from MGMA.
September 2021
Remote Monitoring Devices and Apps for Allergy Practice Can Enhance Patient Engagement and Adherence
The availability and use of remote monitoring devices and applications (apps) has expanded exponentially during the COVID-19 pandemic. Education and self-management interventions for asthma and allergic conditions allow patients to play an active role in their care, and have been linked to improvements in medication adherence and asthma control, and decreases in unscheduled office visits.
Digital tools such as disposable rhinoscopes, digital otoscopes and Bluetooth spirometry can be used in the office, during a telehealth visit, at a remote care site or at the patient’s home. Benefits include:
• Patient satisfaction and convenience
• Standardization and quality improvement
• Teaching and replay options
• Information download to the electronic health record
• Additional practice revenue streams
Mobile health (mHealth) applications are widely available in a variety of formats (smartphones, tablets, computers, wearable technology) and are viewed positively by both patients and physicians. Apps offer symptom diaries, personalized action plans, medication reminders, goal setting/behavior change techniques and more.
More information on incorporating remote monitoring devices and mHealth apps into your practice can be found in the following resources:
• Digital Assessment Tools and Remote Monitoring Devices for Allergy Practice (AAAAI Virtual Practice Management Workshop presentation)
• mHealth and Allergy/Immunology (AAAAI article)
• Drive Patient Retention With Remote Patient Monitoring (Physicians Practice article)
• Remote Patient Monitoring: Building a New Outpatient Revenue Stream (Medical Group Management Association article)
August 2021
Chart Note Do’s and Don’ts
The 21st Century Cures Act contained a provision requiring that physicians provide patient access to most types of medical notes. In the past, these notes were primarily filled with medical jargon and served as a way for healthcare team members to communicate about a patient’s care.
A recent small analysis of physician notes in electronic health records has found that some comments included could be stigmatizing and influence the care of the patient. Researchers identified major themes of both negative and positive language found in the chart note. Here are ways to ensure your notes remain clear and non-stigmatizing:
Avoid language that:
• Includes a large amount of medical jargon.
• Questions a patient’s credibility (e.g., the patient “claimed” something).
• Stereotypes by race, social or gender class.
• Expresses disapproval of a patient’s reasoning or self-care.
Include language that:
• Is straightforward and easy to understand by a non-medical professional.
• Acknowledges patient authority for their own decisions.
• Minimizes blame of the individual for their medical condition.
• Contains positive comments related to the patient and the physician’s view of the patient.
Did you miss the 2021 AAAAI Virtual Practice Management Workshop? You can still purchase and view recordings from all 22 sessions, including “Secrets of a Well-Run Allergy Practice,” which includes additional information on preparing effective chart notes.
July 2021
Maintaining the Health and Wellness of Your Practice Team
When asked to identify the biggest source of stress in their life, 60% of Americans named their job, more than family responsibilities, personal health and economic concerns. Minimizing workplace stressors will lead to a healthier, happier and more productive team. Here are some ideas:
• Meet regularly with your team and ask if there are issues or concerns that need to be addressed. Even more importantly, listen to the team and take action to solve problems that have been identified.
• Recalibrate work hours. Allow some staff to work early and others to work later, which can result in expanded office hours for patients, a win-win situation. Can some of your team continue to work from home for part of the week? Physicians can conduct telemedicine visits, while staff can work on insurance verification. Be flexible, monitor regularly and don’t be afraid to make changes to meet the practice’s needs.
• Celebrate the team. Provide a catered lunch or breakfast. Celebrate birthdays and other special occasions. Say “thank you” often.
Want more ideas on how to cultivate a healthy practice team? Register for the 2021 Virtual Practice Management Workshop that will take place July 23-24. Registration closes July 18.
June 2021
Talking to Your Patients About the COVID-19 Vaccine
While the number of adults and adolescents receiving the COVID-19 vaccine continues to climb, many people remain hesitant about it. Studies show that patients trust their personal physicians, and allergists are in a position to explain the intricacies of vaccine development, testing, efficacy and safety.
According to a recent Kaiser Family Foundation survey, these statements were most impactful in encouraging vaccine hesitant individuals to get vaccinated:
• Vaccines are nearly 100% effective at preventing hospitalization and death from COVID-19.
• Scientists have been working on the technology used in the new COVID-19 vaccines for 20 years.
• More than 100,000 people from diverse backgrounds took part in the vaccine trials.
• The vast majority of doctors who have been offered the vaccine have taken it.
• There is no cost to get the vaccine.
Visit the AAAAI COVID-19 resources page for other helpful resources on how to talk to your patients about the vaccine.
May 2021
Planning for the Future of Telemedicine Post-Pandemic
More than a year into the COVID-19 pandemic, allergy practices have embraced telemedicine thanks in part to a relaxation of regulations during the public health emergency (PHE). The PHE is currently in effect until July 21 and the Biden Administration indicated it will most likely be extended through the end of 2021.
Multiple surveys show that patients are extremely satisfied with the convenience and quality of telehealth visits and want to continue them post-pandemic. While AAAAI and other medical organizations are advocating for permanent implementation of many of the relaxed rules, we don’t know which ones will stay and which will be rescinded.
As you’re planning for the future of telemedicine in your allergy practice, keep these considerations in mind:
• Focus on the problem you’re trying to solve rather than the technology, and then use work flow analysis to find the best solution. Read this Medical Group Management Association (MGMA) article on telehealth and COVID-19.
• While it’s good to recognize that a segment of your patient population may not have the technology to access telemedicine, don’t limit access for those patients that do. Whatever solution you use should be simple and easy to access. Access the AAAAI Telemedicine Toolkit.
• Your telemedicine solutions should meet the needs of you and your patients. These may have changed since the beginning of the pandemic and will likely continue to evolve over time. View this video to see what one allergist learned about telemedicine during the pandemic.
For the most up-to-date information on the future of telemedicine and its impact on your allergy practice, register for the AAAAI Virtual Practice Management Workshop, July 23-24.
April 2021
Understanding the New Information Blocking Rules
New information blocking regulations developed as part of the 21st Century Cures Act went into effect on April 5, with the goal of facilitating better and more secure access to electronic health information (EHI). Our advocacy partner, Hart Health Strategies, has developed a detailed overview of the new regulations and their impact on allergy practice. Here are some key highlights:
• Information blocking refers to a practice that is likely to interfere with access, exchange or use of EHI. The rule applies to providers (hospitals/physicians), health IT developers and health information exchanges/networks.
• The types of data subject to the new regulations include patient medical and billing records, and other records used by physicians to make decisions about an individual’s health care. Specific data elements are defined in the United States Core Data for Interoperability (USCDI) v.1 standard.
• There is no requirement to make EHI information available proactively to individuals, but when it is requested the data should be provided in a timely manner.
Access the full Hart Health Strategies briefing document here, and access additional resources on the information blocking regulations here.
March 2021
Successful Practice Transitions: Selling or Closing a Practice
The COVID-19 pandemic has caused many allergists to reassess their practice situation and consider selling or closing a practice.
If You’re Selling
Selling a practice takes a significant amount of planning, and it is important to assemble a team of experts—accountant, lawyer, appraiser, practice management consultant—to help the process go smoothly. Plan as far in advance as possible, and have a timeline for specific tasks.
The value of a practice is determined by tangible assets (equipment, accounts receivable) and “good will,” which can be subjective and is based on variables such as reputation, history and location, and patient base. While establishing the value of a practice can be tricky, here are some ways to boost your practice value:
• Eliminate as much practice debt as possible.
• Hold off on making major technology investments.
• Keep working (to keep revenue up).
• Maintain curb appeal by keeping your website, financial reports, and office aesthetics up to date.
• Maintain strong relationships with referring sources to demonstrate patient base consistency/growth.
If You’re Closing
Once you’re made the decision to close, plan for 3-6 months to complete the process, and establish a firm closing date. Consult with your legal and accounting teams to ensure your plan is complete.
• Review your vendor, service and managed care contracts for notice requirements.
• Notify patients, staff, and your insurance carriers as early as possible (at least 90 days prior to closing).
• Make arrangements for record storage and maintenance according to state regulations.
For more tips on transitioning your practice, view this presentation from the 2017 AAAAI Practice Management Workshop, and read the chapter “What is an A/I Practice Worth” from the AAAAI Practice Management Resource Guide.
For a practice closing checklist, email practicemanagement@aaaai.org.
February 2021
Navigating the Job Market
Finding your first (or second, or third) job can be challenging, especially during a pandemic. As you explore options, make sure you have a clear vision of your priorities so that you find the best fit for you (and your family).
• Family/personal values: Do you want to be near family/friends? Will your spouse/partner be able to find a job? What type of lifestyle do you want/need?
• Type of practice: It used to be academics or private practice, but there are more options now. Telehealth, research, public policy, consulting, or a combination of roles is possible.
• Do your research: Visit practice websites to get a sense of their mission, culture and staff.
• Be flexible: COVID-19 has turned the job market upside down in some cases, but there are still jobs available. Consider your second or third location choices and be patient.
If you’re a fellow-in-training (FIT) looking for your first position post-fellowship:
• Start looking early (spring/summer during your first year of fellowship) and be proactive by reaching out to practices in your target areas. The recruiting process can take months.
• Have a CV/resume ready.
• Once you’ve made the connection, keep in touch with the practice and continue to show interest.
Here are some additional resources available from AAAAI:
• Chat with Practice Management Committee member Vivian Hernandez-Trujillo, MD, FAAAAI, about navigating the job market in the Practice Management Hub during the AAAAI Virtual Annual Meeting on Saturday, February 27 from 3:15 to 3:45 pm CST.
• Practice Management Basics for the New Allergist: What You Need to Know Before You Start Practice (This webinar recording is free for FIT and NAIA members. Simply email practicemanagement@aaaai.org for the coupon code.)
• View the 2019 FIT exit survey data. You can also find surveys from earlier years here.
January 2021
Managing Your Pandemic Financial Assistance
Did your practice receive financial assistance through the Paycheck Protection Program (PPP) or the Provider Relief Fund (PRF) during the pandemic? Make sure you are aware of appropriate reporting requirements related to the PRF and new opportunities for funds from the PPP so you can plan accordingly.
The PPP was established to help practices cover payroll and other associated expenses, such as group healthcare payments. The initial application deadline was August 8, 2020, but the 2021 Consolidated Appropriations Act recently reopened applications, added additional funding, and made substantive changes to the program, including creating the ability for some borrowers to receive second draw loans if they meet certain requirements. Applications are being accepted on a first-come, first-served basis through March 31, 2021.
For PRFs allocated through the CARES Act, be aware that the reporting portal opened for registration only on January 15, 2021. Given the delay in full functionality, the February 15 deadline has been removed, and the Department of Health and Human Services (HHS) will provide a future announcement regarding updated timelines. Updated PRF FAQs can be found on the HHS site.
The 2020 AAAAI Virtual Practice Management Workshop webinar recordings include an overview of federal pandemic funding from our advocacy partners Hart Health Strategies, and are available free of charge to AAAAI members and their practice staff.
December 2020
COVID-19 Vaccine and Your Staff
Early this month, the CDC’s Advisory Committee on Immunization Practices recommended that healthcare workers be first in line for the initial doses of the COVID-19 vaccine. With an EUA already issued for the Pfizer-BioNTech vaccine and an EUA for the Moderna vaccine expected soon, your practice should already be planning for whether and how to vaccinate your team.
Each state is responsible for allocating the first vaccine doses, and your state public health department website is the best source of information for how to obtain the vaccine and when doses are expected to be available.
Will you require or merely encourage your practice team to receive the COVID-19 vaccination? This article from the Medical Group Management Association (MGMA) is a good overview of practical and legal considerations to help you make the best decision for your practice.
Visit the AAAAI COVID-19 resources page for the latest updates on vaccines, treatments, and other information affecting allergy practice.
November 2020
Protect Your Practice From Cyber Attacks
The FBI and other federal agencies are warning of increased cyber attacks on hospitals and physician practices. In particular, cyber criminals have been sending emails with attachments and links that launch ransomware when clicked. Practices need to remain vigilant with emails from unexpected sources that include links and attachments, particularly those referencing COVID-19. Several resources are available to physician practices:
• American Medical Association (AMA) physician cybersecurity resources
• Department of Health and Human Services (HHS) Health Sector Cybersecurity Coordination Center
• Medical Group Management Association (MGMA) cybersecurity action steps
October 2020
Practice Marketing Strategies During a Pandemic
While you are likely seeing a larger number of patients in the office than you were a few months ago, your practice may still not be at full capacity. Here are some strategies you can use to increase patient volume (both in person and via telehealth):
• Proactively reach out to reschedule visits that were cancelled in the early weeks of the pandemic, and include clear messaging about your COVID-19 safety protocols. Remind patients that you can see them using telemedicine if that is most convenient for them (the public health emergency has been extended until January 23, 2021).
• Keep your practice website up-to-date and prominently feature your COVID-19 safety protocols on the homepage.
• Create a video message on COVID-19 safety protocols for your practice website and send an email to all current patients with a link to the video.
• Develop regular social media posts that keep your practice in the minds of your patients and expand your practice’s visibility within the community.
• Consider purchasing advertising on Facebook, Google, Instagram and other social networking sites.
• Reach out to your referring physicians to see how they are doing and remind them that your office is open and accepting new patients.
The next 2020 Virtual Practice Management Workshop webinar will focus in part on pandemic marketing strategies and is scheduled for Thursday, October 22 from 7:30 to 9:00 pm CDT. Register for the webinar here.
September 2020
Managing Your Practice Cash Flow During COVID-19
The ongoing pandemic is forcing practices to continue to look for strategic ways to ensure their financial health. During the recent 2020 Virtual Practice Management Workshop webinar titled Engineering Your Practice for the Continuing Crisis, panelists provided practical ideas in several areas.
Practice Overhead
• Critically assess your expenses and find places to make permanent or temporary cuts. Do you really need five phone lines? If you have multiple clinic sites, determine which are essential and which can be closed temporarily.
• Review standard supply orders. Is your pre-pandemic schedule still appropriate?
• If you have a mortgage, approach your lender to see if you can temporarily suspend payments without significant penalties. If you have leased clinic space, don’t be afraid to ask for contract modifications.
Meeting Patient Needs
• Be flexible. Offer early morning or early evening appointments, telehealth visits, or consider weekends if that is a need for your patients.
• Be creative with your schedule and give front desk personnel the ability to change appointment types as necessary. Maximizing your ability to see new patients will optimize practice income.
Staffing
• Critically review your staffing levels and assignments and determine if you are right-sized. Cross train staff.
• Ask your nurse practitioners (NPs) to take on additional lower level nursing duties temporarily.
• Determine if some of your staff are willing to work fewer hours on a temporary basis.
Panelists agreed that the bottom line is to remain positive and be flexible and remember that the pandemic won’t last forever. You can access the full webinar recording here.
August 2020
Navigating Staffing Challenges During COVID-19
Is your practice prepared to respond to unexpected staff or provider absences due to COVID-19? In addition to absences due to COVID-19 infection or exposure, many parents will now be faced with how to manage children who will be learning virtually instead of returning to school this fall. Here are some things to consider:
• Cross-train team members as fully as possible to allow for emergency coverage when necessary.
• For staff that are able to work remotely, make sure they are set up to do so. Clearly communicate expectations related to productivity and work hours.
• Manage patient volume by proactively messaging patients scheduled for in-office visits, and reschedule visits via telemedicine if necessary.
• Stay in contact with local temp agencies if some positions can be filled with a temporary worker.
For more ideas on staffing challenges and other COVID-19 issues, register for the next AAAAI Virtual Practice Management Workshop webinar, Engineering Your Practice for the Continuing Crisis, on Thursday, August 27 at 7:30 pm CDT.
July 2020
Communicating With Your Patients Is Critical During COVID-19
Your patients continue to be bombarded with information on COVID-19 daily, and many may still be confused about how to safely manage their allergic disease in face of the continually changing information. They will look to you for guidance on how to minimize risk, and determine which information sources are credible and which are suspect. Here are a few ideas:
• Make sure all of your practice’s COVID-19 precautions and requirements are prominently displayed on the homepage of your website, and communicated via text, email or phone call before the patient’s appointment. This will help calm fears about the safety of visiting the office.
• Continue utilizing telemedicine visits for appointments when appropriate. This helps reduce the number of people in the office and reduce the volume of PPE needed for your staff. Some patients may prefer telemedicine visits to in-person visits and will appreciate having this option.
• Provide your patients with information from credible sources, such as the Centers for Disease Control and Prevention (CDC), World Health Organization (WHO) and AAAAI, and link to these resources from your practice website or provide any available handouts with the information.
Be sure to visit the AAAAI COVID-19 resources page for up-to-the-minute information, like our new patient handout on wearing a face covering or mask, which is available in English and Spanish.
June 2020
Conducting Penicillin Testing With Telehealth
During the COVID-19 pandemic, allergists’ use of telemedicine has expanded significantly, and a large percentage expect to continue utilizing telemedicine even as patients return to the office. A new video lecture titled “Drug Allergy Assessment Using Telemedicine and Electronic Consultations” provides guidance on how to virtually evaluate drug allergy in both in-patient and outpatient settings. This allows for:
• Significant cost savings per patient, including both antibiotic cost and A/I physician time
• Limited in-patient traffic during the COVID-19 pandemic
• Continued de-labeling of penicillin allergy, to further antibiotic stewardship and reduce antimicrobial resistance
View the video lecture or visit the AAAAI penicillin allergy testing advocacy page for more information.
May 2020
Resuming Allergy Practice
As stay at home restrictions begin to ease and your patient volume increases, make sure your office has protocols in place to ensure the safety of staff, patients, and physicians.
The AAAAI COVID-19 Response Task Force has created a list of Suggestions or Considerations for Resuming Practices that includes staff safety protocols, practice space logistics, and a classification of low, medium and high-risk procedures. These suggestions presume that the actual infectious state of your patients is unknown and that asymptomatic or pre-symptomatic patients can spread the virus.
April 2020
Taking Care of Yourself During COVID-19
This is a stressful time. You’re doing your best to keep your patients, staff, family and yourself safe and healthy. You’re using new tools, like telemedicine, in day to day practice. You’re working to ensure the economic impact of the pandemic on your practice and your staff is limited.
During this difficult time, it’s important to remember to take care of yourself, so that you can take care of others.
• Read the article Clinician Wellness During the COVID-19 Pandemic: Extraordinary Times and Unusual Challenges for the Allergist/Immunologist for specific strategies during this uncertain time.
• Watch this new video from the AAAAI wellness group.
• Consider using a mindfulness or meditation app regularly. Some options are:
o Art of Living – Online Happiness Program for Healthcare Workers
o Headspace
o Ten Percent Happier
• Check out the AAAAI physician wellness toolkit for a broader array of ideas and resources.
Visit the AAAAI COVID-19 resources page regularly for updated information to help you and your practice navigate the quickly changing situation.
March 2020
Certain HIPAA Provision Not Enforced for Telemedicine Due to COVID-19
During the COVID-19 national emergency, certain provisions of HIPAA will not be enforced for covered healthcare providers utilizing telehealth services.
Read the announcement, and visit our COVID-19 resources page for further telemedicine resources.
February 2020
Be Aware of In Vitro Allergy Testing Reimbursement Limitations
Recent review of payer policies on in vitro allergy testing reveals several limitations to using these tests in lieu of or in addition to skin testing. Be sure to document in the medical record why you are doing such testing instead of skin tests or in addition to skin tests. If the payer decides not to pay, the patient may come to you for reimbursement unless you have them sign an Advanced Beneficiary Notice. Also, you should be aware of the annual limits that insurers put on these tests (usually in the 20-25 test range, but sometimes up to 35).
January 2020
Ease Prior Authorization Headaches
Navigating prior authorization (PA) requirements is complicated and time consuming. Here are a few ways to minimize the burden:
• Anticipate which medications trigger the highest percentage of PAs and have a plan in place. Can you substitute a generic or other medication that doesn’t require a PA?
• Maintain a series of templates for your most commonly used medications and procedures that require prior authorization so you don’t reinvent the wheel each time.
• Designate a staff person (or a small staff team) to focus on PA rules that can serve as a resource for everyone in the practice.
• Customize your EHR software to alert you when a PA may be required, and take advantage of electronic submission portals when they’re available.
The American Medical Association offers a prior authorization tool kit, including videos and a downloadable tip guide.
The 2020 AAAAI Practice Management Workshop, July 17-19 in Washington, DC, will feature a session on “Prior Authorizations and Other Practice Headaches: Tips and Tricks that Work.” Get more information here.
December 2019
Is 2020 the Year to Implement Telemedicine in Your Practice?
Support for and interest in remote healthcare visits by patients across the entire age spectrum has increased significantly in the last year. Improved technologies, lower costs and increased reimbursement for telemedicine visits could mean now is the right time for your practice to consider implementing these services.
Interested, but not sure where to start? Check out our helpful resources.
• The AAAAI Telemedicine Toolkit offers guidance on a full range of issues including reimbursement, privacy considerations, documentation and more.
• The November/December issue of The Journal of Allergy and Clinical Immunology: In Practice is devoted to telemedicine and electronic applications in allergy and asthma.
• Register to attend the 2020 AAAAI Annual Meeting, March 13-16 in Philadelphia, which will feature several sessions on telemedicine and technology, including a hands-on training station.
November 2019
Managing Penicillin Allergy Testing in Your Practice
One of the primary ways to combat antimicrobial resistance begins with penicillin. Approximately 10% of the U.S. population thinks they are allergic to penicillin, yet 9 out of 10 are not truly allergic when formally tested. This provides a significant opportunity for allergy practices, and the AAAAI has several resources to help you manage the penicillin testing process:
• Optimal coding strategies for penicillin allergy testing
• Sample protocols and documentation for challenge testing from the 2019 AAAAI Practice Management Workshop
• AAAAI Penicillin Toolbox
• Information on AAAAI advocacy efforts on penicillin testing, policy statements, and patient education resources
October 2019
Is It Time to Stop Calling Your Patients?
How much time does your staff spend calling patients to remind them about appointments, provide lab results and verify insurance coverage, only to end up leaving voicemails and playing phone tag? If you’re looking for a more efficient (and effective) way to communicate, consider texting your patients. Recent studies show:
• 95% of your patients own cell phones, including 91% of adults 65 and older.
• 98% of texts are read, 95% of them within 3 minutes.
• Most Americans would rather receive a text than a phone call, and more than 30% of voicemail messages go unheard for three days or more.
Text messages can be used as reminders, to provide education after the visit, or to increase compliance and adherence. Texts can also be used to provide updates on unexpected schedule changes (for example, a blizzard forces you to close the office for the day). For more on effective patient communication strategies, read this blog post from Physicians Practice.
September 2019
Getting Approvals for Immunoglobulin and Other Biologic Therapies
Obtaining insurance company approvals for immunoglobulin (IG) therapy is, for many physicians, among the most unpleasant aspects of patient care. Here are some tips for simplifying the process that have been shown to routinely result in gaining the required approvals.
Before You Start
It is crucially important to know the ground rules for IG therapy in PIDD both generally and in relation to the specific insurer. Particular payers often consider particular diagnosis codes to be supportive of the need for IG and other codes not. If you use the wrong code, there will be an immediate denial. Now that some payers are using preferred drug lists (PDLs) limiting the options with regard to brand, you must know the payer’s PDL as well. Usually, this information is available on the payer website or from the payer provider rep, but sometimes the payer keeps it a secret requiring the physician to make their best guess.
It goes without saying that it will be easier to get an approval for a patient who clearly meets clinical and laboratory criteria for IG therapy. Before you start your letter, you should be familiar with your patient’s history, particularly significant events like an episode of meningitis or osteomyelitis and have relevant diagnostic labs compiled. You should also be clear about the IG product and mode of administration you want to use.
Writing the Letter
Start the letter by saying what you want, for example: “I am writing to request authorization for immunoglobulin supplementation therapy for the above referenced patient with a disorder of antibody production. I have recommended intravenous immunoglobulin therapy for this patient.”
Less is more! Keep the IG approval letter to one side of a page and use the same description of the patient’s history, for example: “This patient had a long history of recurrent bacterial respiratory tract infections. An immunologic evaluation demonstrated disorder of antibody production (laboratory studies attached). The specific diagnosis is listed below. Because his infections could not be controlled with the most aggressive conventional therapy, this patient needs immunoglobulin supplementation therapy.”
List the ICD-10 code and its description, the specific product name with its J code followed by the dose in grams and the infusion mode and interval. Here’s an example with each of these elements printed in bold on a separate line*:
D80.0 – X-Linked agammaglobulinemia, autosomal recessive agammaglobulinemia, hypogammaglobulinemia
Drug: Carimune J1566
Dose: 30 grams
Interval: every four weeks
Enclose copies of the diagnostic supporting lab studies with the letter.
A similar approach can be utilized for omalizumab for asthma, beginning the letter with a brief description of criteria (e.g., moderate to severe asthma), the last weight and IgE level and their dates, and closing with the dose (in vials and milligrams) and interval.
*This example uses a drug name and J code that is no longer on the market to avoid promoting a particular brand.
August 2019
Take Control of Your EHR
As of 2017, 86% of office-based physicians had adopted an electronic health record (EHR). Since 2008, this has more than doubled, from 42% to 86%. While the promise of EHRs was to improve our access to patient data and streamline ordering and billing, increasing evidence suggests it is making our work day more difficult. A study published this past year found that the use of EHRs contributes significantly to physician stress and burnout, adding to our daily frustration level. Physicians also reported having inadequate time for documentation and spending large amounts of time working on EHRs at home. It is not too late to optimize your current EHR.
1. Ensure you are up to date on your version of your EHR. While upgrading may seem laborious and unnecessary, upgrades are usually better versions, often with additions recommended by providers. This also ensures ongoing interoperability with your practice management software and other IT tools.
2. Ensure adequate training after upgrades. The amount of training providers get on their EHR correlates with satisfaction levels. This is not only true during initial instillation but also for upgrades. Have a “provider champion” review the upgrade notes and share the info with all the providers.
3. Ensure your clinical workflow takes advantage of your EHR capabilities. Maximize the amount of information your front desk, then medical assistant or nurse can enter into the EHR before sending the patient chart to you. Document as much of the chart note as you can while the patient is still in the office, leaving less to have to go back to later.
4. Let individual providers adapt processes that work best for them. Not everyone has to do it the same way. Some providers may do better typing their notes into the EHR, some may prefer to dictate parts or all of their notes, and some may do better with a medical scribe.
Ongoing optimization can be crucial to keep your EHR working for you.
Resources:
Percentage of office-based physicians using any electronic health record (EHR)/electronic medical record (EMR) system and physicians that have a certified EHR/EMR system, by U.S. state: National Electronic Health Records Survey, 2017 pdf icon[PDF – 371 KB]
Rebekah L Gardner, Emily Cooper, Jacqueline Haskell, Daniel A Harris, Sara Poplau, Philip J Kroth, Mark Linzer, Physician stress and burnout: the impact of health information technology, Journal of the American Medical Informatics Association, Volume 26, Issue 2, February 2019, Pages 106–114.
Monica Kate. 11 Ways Medical Practices Can Get More Out of Their EHR Systems. Accessed 28 July 2019
July 2019
Hiring the Right Staff for Your Practice
Your patients’ perceptions of your allergy practice depend not just on the care provided by the physician, but also on their interactions with your practice staff, from the front desk to the MA to the nurse. How can you ensure you’re hiring (and keeping) high quality staff?
• Make sure the job description is up to date and potential employees are clear on expectations and responsibilities.
• Review applications carefully to ensure applicants have the right experience and training, and don’t be afraid to contact references.
• Ask open ended questions during the interview, and if possible, have the final candidate spend a couple of hours shadowing staff in the practice.
• Once hired, make sure the new employee gets a thorough orientation to the job and the practice.
For more insights on hiring the right staff for your practice, pre-order the recordings from the 2019 Practice Management Workshop, or read the chapter on Staffing and Human Resources Issues in the Practice Management Resource Guide.
June 2019
Implementing the New USP 797 Standards in Your Practice
New USP Chapter 797 standards on sterile compounding were released June 1 and take effect December 1. Practices have the option of preparing extracts using an ISO Class 5 Primary Engineering Control (PEC) OR in a dedicated Allergenic Extracts Compounding Area (AECA). Additional personnel qualifications and training is also required to be in compliance.
The AAAAI website has a variety of resources to help your practice meet these standards, including:
• An overview of the new standards and requirements for allergy practice compounding areas
• Personnel qualifications, hygiene and training requirements
• A podcast episode with Andrew W. Murphy, MD, FAAAAI, where he breaks it all down and provides background, details about Chapter 797, and tips for implementation
The AAAAI Practice Management Workshop, July 12-14 in Cincinnati, will feature an expert session on implementing the new USP 797 standards in your practice, along with other important practice management topics. Online registration is open through July 1.
May 2019
HIPAA for the Practicing Allergist
HIPAA is an acronym for the Health Insurance Portability and Accountability Act of 1996. “Privacy” and “Security” are not in the name HIPAA, but they present our biggest challenges.
The Office of Civil Rights revenue from HIPAA violations has doubled every year since 2012. Practices of all sizes are at risk, but smaller size practices are at higher risk. The practice or business can be fined for HIPAA violations even if a breach doesn’t occur. That is the case when a Business Associate does not comply with the HIPAA rules.
Business Associates (BAs) are individuals or entities who create, receive, maintain, or store private health information on behalf of a covered entity. Answering services, medical transcription, IT groups, billing companies, and shredding services are considered BAs.
HIPAA requires that BAs must now:
• develop policies and procedures for HIPAA, as well as train staff
• conduct risk analysis
• be subject to federal inspections
• monitor covered entities where a Business Associate Agreement exists and have Business Associate Agreements with sub-contractors
• be subject to the HIPAA Breach Notification Rule
In 2019 the major issue is communicating with patients and providers utilizing emails and text messaging while complying with the HIPAA rules.
To learn more, attend the 2019 Practice Management Workshop, July 12-14 in Cincinnati, Ohio.
April 2019
Be Aware of Insurer Skin Testing Limits
Insurers are beginning to limit the number of skin tests a patient may have over a period of years (the time varies with insurer). If your new patient has had previous testing, you may not get paid. Be sure to familiarize yourself with the limitations of your most prevalent insurers so you are not surprised! The AAAAI Office of Practice Management is working with insurers to make sure that these limitations are reasonable. For example, there should be no skin test restrictions when a patient is changing allergists.
Click here for more information on additional AAAAI advocacy activities.
Looking for other great practice management ideas? Register for the 2019 AAAAI Practice Management Workshop, July 12-14 in Cincinnati, Ohio.
March 2019
Don’t Be Afraid to Negotiate Your Employment Contract
Whether you’re starting your first job after fellowship or are well into your allergy career, you can successfully negotiate (or renegotiate) your employment contract. Here’s how to start:
• Read up on negotiation strategies and practice your pitch.
• Research the market value for allergists in your area so that you have an idea of what you can reasonably expect.
• Remember that base salary is only part of your overall compensation package, which can include benefits like health, malpractice and life insurance, paid time off, CME days/CME allowance, relocation or moving allowances, and more.
The AAAAI Practice Management Resource Guide has more specific information on contract negotiation strategies, and this post on the KevinMD blog includes some great ideas for how to determine your market value.
Early career allergists can learn contract negotiation strategies from seasoned employment attorney Penny Phillips, JD, at the 2019 AAAAI Practice Management Workshop, July 12-14 in Cincinnati, Ohio.
February 2019
Payer Relations
Many insurers are requiring proof of reversibility of airway obstruction for the approval of biologics. By the time the patient needs biologics, however, documenting reversibility may be difficult.
Remember to be sure that this test is performed at some point early in the course of asthma, if appropriate, so you have documentation when the time arrives. The AAAAI Office of Practice Management is corresponding with these insurers about the practicality of this requirement.
January 2019
Successful Practice Transitions
With increasing mandates and complexities of practice, many physicians are either selling or closing a practice or joining larger entities in order to reduce financial and administrative burdens. Here are some things to consider if you’re:
Selling your practice
- Plan as far in advance as possible, and have a timeline for specific tasks.
- Assemble a team of experts – accountant, lawyer, appraiser – to help the sale go smoothly.
- Eliminate as much practice debt as possible, and hold off on making major technology investments.
Closing your practice
- Review your vendor, service and managed care contracts for notice requirements.
- Notify patients, staff and your insurance carriers as early as possible (at least 90 days prior to closing).
- Make arrangements for record storage and maintenance according to state regulations.
For more tips on transitioning your practice, view this presentation from the 2017 AAAAI Practice Management Workshop.
December 2018
Start the New Year Off on the Right Financial Foot
Get yourself and your practice off to a good start in the new year by taking some time to think about your financial goals now.
For Yourself
Physicians start their first real job relatively late in life, and many have little or no financial experience and a significant debt load. It’s never too early (or too late) to get yourself on the track to fiscal fitness:
• Live below your means. Aim to save 15% of your gross income every month and set up a sensible household budget that covers your needs and wants. Consider buying a smaller house or less expensive vehicle until you are financially well-off.
• Build an emergency fund, then prioritize paying down debt (higher interest rate loans first).
• Whenever possible, use low cost, index mutual funds to invest.
• Diversify your investments to include an appropriate allocation of stocks and bonds, and make sure you are investing appropriately for your age and risk tolerance.
• Never try to time the market. Rather, periodically rebalance your portfolio to ensure that your desired asset allocation is maintained.
• Maximize your tax efficiency. Take advantage of tax-deferred plans like 401(k), 403(b), IRAs, 529s and HSA accounts. These allow your investments to grow tax-free.
For Your Practice
• Do you have patients with high deductible health plans (HDHPs)? Consider utilizing a credit card on file to automatically collect payment at time of service, or use them for monthly budget payment plans.
• Review your payer contracts and update your fee schedule annually. Keep a master list of your payers and their allowed charges to help you identify potential problems early.
For more financial tips, view these presentations from previous AAAAI Practice Management Workshops:
Revenue Cycle Management: From Appointment to Payment and Beyond
Personal Finances and Investing for the Physician: A Boglehead’s Approach
November 2018
Do You Know Your Practice Culture?
Studies show that a high performing medical practice with a strong culture:
• Can adapt more easily to changes in the marketplace
• Has employees who are more engaged, productive and aligned with the practice mission
• Benefits from lower employee turnover and less stress and burnout among physicians and staff
All of these factors contribute to higher patient satisfaction and a better bottom line for the practice. For more information on how to assess and improve your practice culture, view these slides from the 2016 AAAAI Practice Management Workshop.
October 2018
Is Your Practice Prepared for an Audit?
Today, it’s a matter of when, not if, your practice will be audited. While audits can be nerve-wracking, there are things you can do now to ensure your practice is prepared for the inevitable.
• Keep meticulous records of your expenditures. File them on a regular basis (preferably monthly) and store them by calendar year. This will make it easy for you to assemble documentation quickly for the auditor.
• Create a checklist for your financial activities, from front desk collections to tax filing procedures. Make sure the staff responsible for these activities follow the checklist, and train new staff in your procedures as part of your onboarding system.
• Keep personal and business accounts separate.
For more practical details, listen to A Step by Step Guide to Surviving Practice Financial Audits from the 2018 AAAAI Practice Management Workshop.
SEPTEMBER 2018
Disaster-Proof Your Practice
Extreme weather events such as hurricanes, tornados, floods and wildfires are occurring at an increased rate. Is your practice positioned to weather the storm? Here are some lessons learned by Coastal Allergy & Asthma in Savannah, Georgia after Hurricane Matthew:
• Have a written disaster plan/procedure and make sure your staff is familiar with it. When emergencies arise, initiate your plan to ensure the safety and well-being of practice staff and patients.
• Closely review your business interruption insurance policy to make sure it will cover your operating expenses in the case of an unexpected shut down. It is also important to know what events trigger the insurance. As Coastal Allergy & Asthma found out, a mandatory evacuation order for an impending hurricane was not enough.
• Make sure you have a back-up generator in case of power failure and know how to start it manually.
• After the disaster, carefully inspect your property for potential damage.
Get more disaster preparedness tips and a sample plan here.
August 2018
Does Cyber Insurance Make Sense for My Practice?
Allergy practices are experiencing escalating day-to-day operating expenses, but one expense we may no longer want to delay is the purchase of cyber insurance. In a 2017 survey by the American Medical Association and Accenture, 83% of physicians reported experiencing some sort of cyber attack. An accidental or deliberate patient data breach can cost your practice over $100,000 plus penalties.
What does one need to look for in a cyber policy? There are key categories that seem to be standardized in each cyber policy, but a comprehensive policy will cover losses resulting from patient data being stolen, exposed or improperly shared. It will cover breaches from deliberate actions, such as hacking or ransomware, as well as accidents (such as a lost laptop containing unencrypted patient data). You’ll want to sit down with your insurance broker and compare policies side by side to determine which option is the most cost effective for your practice.
Looking for more practice tips? Order the recordings from the 2018 Practice Management Workshop. Topics include billing, coding, financial benchmarking and more.
July 2018
Maximize Your Revenue by Avoiding Common Billing Blunders
Conducting an annual audit of your practice’s revenue cycle management processes will help you avoid costly errors that can negatively impact your collections. Make sure to:
• Determine the patient’s benefits prior to the appointment (when possible) and collect co-payments at the time of the visit (always).
• Review all insurance payment guidelines at least every 6 months to ensure you are submitting appropriate and timely documentation for claims. This will decrease denials and staff time required to file appeals.
• Code each patient encounter appropriately, to the highest level of service supported by documentation.
AAAAI coding consultant Teresa Thompson and Tessie Adams will be reviewing these tips and more at the 2018 AAAAI Practice Management Workshop in Salt Lake City during their session “Beyond Correct Coding: Getting Paid for What You Do and Avoiding Billing Blunders.” Can’t make it out to Salt Lake City for the workshop? Preorder the recordings here.
June 2018
Implementing Telemedicine into Your Practice
Have you seen a decline in growth in your practice? Telemedicine may help increase that growth with some considerations.
• Decide what the best work flow may be for your practice, whether it’s practicing telemedicine one day a week, in between in-person consultations or something else.
• If you implement telemedicine it must be secure and compliant with state and federal regulations.
• It is important to confirm that medical liability coverage includes a provision for telemedicine services.
• You don’t want to water down your current level of care so ensure your live interactive video visits with patients be at the same standard of care, professionalism and ethics as your in-person consultations.
For more tips on incorporating telemedicine into your practice, register for the 2018 Practice Management Workshop, July 20-22 in Salt Lake City, Utah.
May 2018
Navigating the Solo Allergy Practice
Although the majority of fellows-in-training and young physicians join existing single specialty and multispecialty groups as well as academic institutes, a number of new grads are either considering or have already started solo practices. If you are in solo practice or considering solo practice, these tips are for you.
1. The stability and survival of a medical practice depends on its financial success. And the financial success depends on having a steady flow of patients, providing excellent patient care, good management and controlling the overhead while delivering the best care. Recruiting patients in solo practice is highly dependent on the physician’s reputation, which is in contrast to group practices where the flow of patients is greatly influenced by the reputation of the group or senior partners. To this end:
- Make sure your patients are having a great experience when they visit your office from scheduling to billing and collection.
- Learn appropriate scheduling to avoid having patients wait in the exam rooms or waiting room more than 10 minutes to see you.
- Listen and address patients’ concerns.
- Explain why you are doing any investigations or testing.
- Involve your patients in the decision making regarding treatment options and remember: satisfied patients are the best free advertisement for your practice.
2. When seeing a patient, communicate with the primary care provider even if the patient was not referred to see you.
3. Don’t speak negatively about other physicians. Not only it is unprofessional, but patients will not respect you or your medical opinion.
4. Hiring an experienced practice manager may not be financially feasible in first 5 to 7 years of practice and in some instances might discourage you from learning how to manage a practice. Consider hiring an assistant manager or attending the annual AAAAI Practice Management Workshop. The workshop will provide you with tools to understand all aspects of hiring, training and retaining staff, as well as scheduling, billing and understanding financial benchmarks. You also have the opportunity to network with a large group of allergy/immunology physicians and office managers with a wide range of expertise.
April 2018
Utilizing Nurse Practitioners and Physician Assistants in an Allergy Practice
Are you considering hiring a nurse practitioner (NP) and/or physician assistant (PA) in your practice? Adding an NP or PA can:
• Expand physician schedule capacity
• Generate additional practice revenue
• Allow quicker access for acute visit patients
At Allergy, Asthma & Immunology Center of Alaska, one NP and one PA support five allergists at one location, according to Melinda Rathkopf, MD, FAAAAI. “Our NP and PA do routine follow-up visits (like annual immunotherapy visits), not new patient visits. They often have more availability to see acute visits quickly and are the first to respond to shot room reactions. They are an invaluable addition to our clinic and allow the allergists to focus on more complex patients.”
To ensure a good fit for your practice, you’ll want to assess if the NP or PA candidate shares your practice philosophy and is able to collaborate and adapt to your style of medicine.
For more tips on incorporating an NP or PA into your practice, view this presentation from the 2016 AAAAI Practice Management Workshop or register for the 2018 workshop, July 20-22 in Salt Lake City, Utah.
March 2018
Physician Wellness
Given the current and future healthcare climate, physician health and wellness is and will remain a significant issue. Here are some tips for the individual physician to help improve wellness and reduce burnout:
• Take care of yourself. Physicians are often involved in taking care of family members, including spouses and children, in addition to treating patients. Maintaining adequate sleep, nutrition and exercise is important, as is making sure to address your own physical and emotional issues by regularly seeing healthcare providers.
• Find a sanctuary outside of medicine. Take up a hobby or volunteer for a cause you believe in to help alleviate the daily stresses of practice.
• Take your scheduled vacation time to destress and allow a “recharge” of energy. Many physicians do not fully use their allotted vacation times.
• Take small breaks during the work day, including breaks from electronic devices.
• Focus on the positive aspects of work as well as family and personal issues, and maintain a sense of humor regarding these topics.
Remember, as healthier allergists/immunologists, we can be even better advocates for our patients and our wonderful specialty.
Reference: Nanda A, Wasan A, Sussman J. Provider Health and Wellness. J Allergy Clin Immunol Pract 2017; 5: 1543-8.
February 2018
Sample Anti-Harassment Statement and Policy
Sexual harassment allegations have made the news repeatedly in the last few months. The AAAAI has added a sample anti-harassment statement and policy here for your consideration, but remember to always consult legal counsel in your own state before adopting any new policies and procedures in your practice.
Looking for more ways to improve your practice? Select recordings from the 2017 Practice Management Workshop are available for purchase in the AAAAI Continuing Education Center. Registration for the 2018 Practice Management Workshop, July 20-22 in Salt Lake City, Utah, will open March 1.
January 2018
Use Social Media to Engage with your Patients and your Community
A recent Google Think survey found over 76% of patients were getting their healthcare information online. Make sure your practice website is up-to-date and engaging, and then leverage other social media platforms to engage with your patients and your community.
• Facebook: Establish a Facebook page for your practice and post information regularly (weekly, at a minimum, is best). Ask patients to “like” your practice page. Keep your personal Facebook page separate and don’t accept “friend” requests from patients.
• Twitter: Why Tweet? It’s a real time network with more than 328 million monthly active users. Use Twitter to communicate simple messages like pollen counts, shot hours and office hour changes. Build up a network of followers and connect with other allergists on Twitter.
• YouTube: This video sharing site can help you market your practice. Post short videos on key allergy topics, procedures (patch testing, etc.), or to answer common patient questions. You don’t need expensive equipment. You can use your smartphone to record and upload the video.
Find more tips on our Social Media 101 page, or Take a look at the slides from the 2017 Practice Management Workshop session on new practice marketing techniques. (Only AAAAI members can access this document.)
December 2017
Do You Need an Employee Handbook?
An employee handbook is needed whether you are a solo physician, practicing in a single specialty or part of a multispecialty group. It is the document that will provide your employees with the proper guidelines and rules that govern your practice and will allow you to reward or discipline an employee when needed. Fair employee treatment cultivates loyal employees. The employee handbook should include the following:
1. Mission and vision of the practice. It’s important to invest in developing a mission and vision that reflects your goals and beliefs and fits your practice style. Great mission and vision statements will motivate your staff.
2. Job titles and descriptions for all categories of the office staff.
3. The office hours of the practice.
4. What constitutes part-time and full-time employment and what benefits each are entitled to receive.
5. An outline of all benefits (medical and dental insurance, life insurance, CME allowance, PTO) and how to qualify for them.
6. A description of what actions result in disciplinary actions, as well as steps for disciplinary actions.
7. Rules about use of cell phones during office hours and personal use of office computers.
8. A statement and mandatory education on the Health Insurance Portability and Accountability Act (HIPAA) including the consequences of HIPAA violations.
9. Your sexual harassment policy, including your complaint or investigation procedure.
Employees must read the handbook and sign an acknowledgment that they read it. The signed acknowledgement should be page kept in each employee’s file.
Looking for more ways to improve your practice? Select recordings from the 2017 Practice Management Workshop are available for purchase in the AAAAI Continuing Education Center. Registration for the 2018 Practice Management Workshop, July 20-22 in Salt Lake City, Utah, will open in March.
November 2017
Negotiating Managed Care Contracts
Is your practice experiencing declining reimbursements? Here are some tips consultant Ron Howrigon shared during the 2017 Practice Management Workshop:
• Negotiation is a process, not an event. Your first plan generally won’t survive the first round; be prepared to adapt, adjust and overcome.
• Set goals for your negotiation. Reimbursement rates are essential, but contract language can be just as important. Set your opening position, identify areas open for negotiation and be clear on your walk away points.
• Knowledge, analysis and planning are essential for a successful negotiation. To strengthen your position, make sure you:
- Create a master fee schedule of each payer’s reimbursement level.
- Know your payer mix. How hard do you want to negotiate with a company that is only responsible for 6% of your payments?
- Know your contracts. Create a contract summary form that includes the fee schedule, effective dates, contract point outliers, etc. for each payer.
This session and other select recordings from the 2017 Practice Management Workshop are available for purchase in the AAAAI Continuing Education Center. Mark your calendar for the 2018 Practice Management Workshop, July 20-22, in Salt Lake City, Utah.
October 2017
Reducing Physician Burnout
Physician burnout can be caused by excessive workload, poor work-life balance and lack of control. Here are some tips from the American Medical Association (AMA) Steps Forward Campaign to reduce physician burnout:
1. Daily huddle with your team: Spend 5 to 10 minutes each day talking to your nurses and other office staff to plan how your day might go. Discuss the scheduled patients who might need more time with the provider or need any labs, tests and records to be retrieved or done before seeing the provider.
2. Have a documentation team: Nearly half of providers say they spend too much time on clerical tasks. Have your nurses help you enter clinical data. Train them to get better on their technology skills. Increasing the number of your support staff might actually save you more money. Consider hiring a medical assistant to serve as your scribe and as your nursing assistant.
3. Better prescription management: When prescribing a medication, consider prescribing a 90 day supply of medicines with 2-4 refills and try to be consistent in doing this. It will reduce the number of calls into your office for refills and other prescription changes. If a patient calls asking for refills, then you and your staff know immediately that a patient has not been to your office in a while and needs a follow up appointment.
Visit the AAAAI Continuing Education Center to order the recordings from the 2017 AAAAI Practice Management Workshop, which includes the topic "Practice Transformation: Reducing Burnout and Rediscovering the Joy in Practice."
September 2017
Handling Biologics in Your Practice
Here are a few tips from the 2017 Practice Management Workshop presentation on How to Handle Biologics in Your Practice:
1. Determine the number of patients that your practice has on biologics. It might be time to assign or hire a person on your staff to solely manage the handling, billing and administration of biologics.
2. Keep a detailed inventory and tracking log, and update it every day. The log should include patient names and insurance and specialty pharmacy information, payment information, dosage, and vials and milligrams used.
3. Do not forget about disaster management. In light of the most recent weather-related disasters, do not forget about having disaster insurance on your inventory of biologics and allergy extracts and vials. Even a simple prolonged power outage can destroy thousands of dollars’ worth of biologics, extracts and medicines.
To learn more tips, the AAAAI is offering select recordings of the 2017 Practice Management Workshop for purchase at the AAAAI Continuing Education Center.
Click here for full issues of Practice Matters!
