COVID-19 and Asthma: What Patients Need to Know
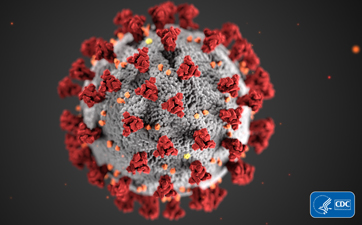 The coronavirus disease 2019 (COVID-19) pandemic is scary for all people, but for those with asthma there is great fear that they will have a worse outcome or be more likely to get SARS-CoV-2 (the virus that causes COVID-19). It is important to know that currently there is no evidence of increased infection rates in those with asthma. And although the Centers for Disease Control and Prevention states that patients with moderate-severe asthma could be at greater risk for more severe disease, there are no published data to support this determination at this time. There have been many studies looking at the relationship between COVID-19 and asthma. Thus far the vast majority of these studies have found no increased risk of COVID-19 disease severity in those with asthma. Further, there appears to be no indication that asthma is a risk factor for developing COVID-19 disease. However, a few studies have suggested that non-allergic asthma may be associated with more severe COVID-19 disease, although it is not clear in these studies that subjects did not have chronic obstructive pulmonary disease (COPD), which is a well-established risk for severe COVID-19. Finally, early data from New York State had suggested a reduced death rate in asthma patients hospitalized with COVID-19, but this has not been reproduced in other studies. Taken together, it appears that there is either no risk or at most a very slight risk for more severe COVID-19 disease in non-allergic asthma patients. This is in contrast to other risk factors like COPD, obesity, etc., that have consistently been linked to more severe COVID-19 disease.
The coronavirus disease 2019 (COVID-19) pandemic is scary for all people, but for those with asthma there is great fear that they will have a worse outcome or be more likely to get SARS-CoV-2 (the virus that causes COVID-19). It is important to know that currently there is no evidence of increased infection rates in those with asthma. And although the Centers for Disease Control and Prevention states that patients with moderate-severe asthma could be at greater risk for more severe disease, there are no published data to support this determination at this time. There have been many studies looking at the relationship between COVID-19 and asthma. Thus far the vast majority of these studies have found no increased risk of COVID-19 disease severity in those with asthma. Further, there appears to be no indication that asthma is a risk factor for developing COVID-19 disease. However, a few studies have suggested that non-allergic asthma may be associated with more severe COVID-19 disease, although it is not clear in these studies that subjects did not have chronic obstructive pulmonary disease (COPD), which is a well-established risk for severe COVID-19. Finally, early data from New York State had suggested a reduced death rate in asthma patients hospitalized with COVID-19, but this has not been reproduced in other studies. Taken together, it appears that there is either no risk or at most a very slight risk for more severe COVID-19 disease in non-allergic asthma patients. This is in contrast to other risk factors like COPD, obesity, etc., that have consistently been linked to more severe COVID-19 disease.
It is worth noting that there are seasonal versions of coronaviruses that have been shown to cause asthma exacerbations. The original SARS-CoV-2 virus (like SARS-CoV and MERS-CoV, the two other pandemic coronaviruses) did not seem to cause asthma exacerbations; however, since the Omicron variant, SARS-CoV-2 has been associated with asthma exacerbations. So, if you have asthma you should treat SARS-CoV-2 like any other respiratory virus that can cause your asthma to flare. Keeping your asthma under the best possible control at all times is the best way to deal with any infection or allergen exposure that leads to an asthma exacerbation.
The bottom line for people with asthma dealing with SARS-CoV-2 is to keep doing what you have been doing all along—continue taking your controller medication and inform your healthcare provider of any symptoms that you may develop. If you have an asthma action plan, be sure to follow it, and of course, remember to wash your hands. To reduce your risk of getting a respiratory infection (not just SARS-CoV-2) you may wish to wear a mask when in large groups during a viral peak. Finally, remember to get your seasonal influenza and SARS-CoV-2 vaccines each year!
1. https://www.nytimes.com/2020/04/16/health/coronavirus-asthma-risk.html
2. Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430-436. doi:10.1038/s41586-020-2521-4
3. Yang JM, Koh HY, Moon SY, et al. Allergic disorders and susceptibility to and severity of COVID-19: A nationwide cohort study [published online ahead of print, 2020 Aug 15]. J Allergy Clin Immunol. 2020;S0091-6749(20)31136-2. doi:10.1016/j.jaci.2020.08.008
4. Gupta S, Hayek SS, Wang W, et al. Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US [published online ahead of print, 2020 Jul 15]. JAMA Intern Med. 2020;e203596. doi:10.1001/jamainternmed.2020.3596
5. Gaietto K, Bergum N, Rosser F, Snyder O, Acevedo-Torres N, DiCicco LA, Butler G, Rauenswinter S, Iagnemma J, Wolfson D, Han YY, Kazmerski TM, Forno E. Odds of COVID-19-associated asthma exacerbations in children higher during Omicron wave. Pediatr Pulmonol. 2023 Nov;58(11):3179-3187. doi: 10.1002/ppul.26642. Epub 2023 Aug 18. PMID: 37594160; PMCID: PMC10592137.
Visit our COVID-19 Resources.
The AAAAI's Find an Allergist / Immunologist service is a trusted resource to help you find a specialist close to home.
1/31/2024