Hives (Urticaria) and Angioedema Overview
 Hives or welts, also known as urticaria, are itchy, raised, reddish areas on the skin. About a quarter of the general population can have hives during their life. Hives often appear without warning and may start at any age.
Hives or welts, also known as urticaria, are itchy, raised, reddish areas on the skin. About a quarter of the general population can have hives during their life. Hives often appear without warning and may start at any age.
Angioedema is swelling below the surface of the skin and fatty tissue. Areas of 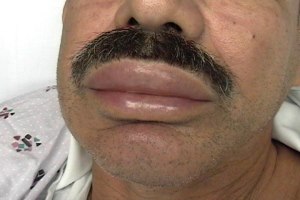 swelling may be painful. Angioedema usually occurs in the face, throat, hands, and feet. Swelling can also occur in the abdomen or other areas of the body. Throat swelling can be life threatening and requires immediate medical attention. It is important to understand that angioedema is a medical term to describe swelling. It can be found with many different disorders. Angioedema can occur with or without hives. There are several different ways swelling can occur. Understanding the underlying mechanism of swelling or the specific disease is critical in determining the best treatment.
swelling may be painful. Angioedema usually occurs in the face, throat, hands, and feet. Swelling can also occur in the abdomen or other areas of the body. Throat swelling can be life threatening and requires immediate medical attention. It is important to understand that angioedema is a medical term to describe swelling. It can be found with many different disorders. Angioedema can occur with or without hives. There are several different ways swelling can occur. Understanding the underlying mechanism of swelling or the specific disease is critical in determining the best treatment.
Hives and Angioedema Symptoms & Diagnosis
Hives:
- are itchy and can occur anywhere on the body including the face, extremities, chest, back or face.
- may range in size from just a few millimeters to several centimeters.
- usually fades individually within a 24-hour period and the skin returns to normal without leaving any marks or bruising.
Doctors will classify your hives based on how long you have had them. This helps doctors think about possible causes of your hives. When hives occur for less than 6 weeks, we call this acute urticaria. When hives last longer than 6 weeks, we change the name to chronic urticaria. Sometimes the hives in chronic urticaria can occur with angioedema (swelling).
There are two types of chronic urticaria: chronic inducible urticaria and spontaneous urticaria. Neither form of Chronic urticaria is dangerous. Chronic inducible urticaria is caused by an environmental trigger such as heat, cold, or pressure applied to the skin. The most common form of the inducible urticarias is called dermatographic urticaria. It can occur in all age groups. Dermatographic urticaria is triggered by shearing forces against the skin such as scratching, pressure from tight clothing resulting in the linear appearing hives. Stroking, or scratching the skin with a firm object will elicit the response in 5-7 minutes. Hives can last for 15 minutes to 3 hours. Antihistamines are frequently an effective form of treatment.Spontaneous remission can occur in 2-3 years.
Usually the cause of chronic spontaneous urticaria is not fully known but is not usually caused by allergies. This is a constant finding of medical authorities and researchers around the world. The absence of an identifiable trigger can be frustrating for patients. Sometimes chronic hives may be autoimmune in nature, or related to an autoimmune condition including autoimmune thyroid disease, rheumatoid arthritis or systemic lupus erythematousus.
Classifications
|
Acute Urticaria
|
Chronic (spontaneous or inducible) Urticaria
|
|
Spontaneous hives, angioedema or both for less than 6 weeks
|
Spontaneous hives, angioedema or both for more than 6 weeks
|
|
Often due to:
• viral infections (most common)
• food allergy
• drug allergy
• environmental allergy
• insect bites
|
Spontaneous hives often have an association with autoimmunity
Inducible urticaria:
Physical Urticaria (non-allergic hives from environmental triggers)
• Scratching/rubbing (dermatagraphic urticaria)
• Pressure/tight clothes (pressure urticaria)
• Sweating/increased temperature (cholinergic urticaria)
• Cold exposure, ice (cold urticaria)
• Swelling from vibration (vibration induced angioedema)
• Sunlight (solar urticaria)
• Water (aquagenic urticaria)
|
Modified from http://www.urtikaria.net/en/forms-of-urticaria/overview.html
Angioedema without Urticaria: A Special Situation
Talk to your doctor if swelling occurs without hives. This may suggest a special situation requiring additional evaluation. Sometimes high dose antihistamines may not improve your swelling. This is because the mechanism (cause) of swelling may be different than that of hives.
Swelling without hives may be due to:
• Aspirin or nonsteroidal anti-inflammatory drug (NSAIDs) such as ibuprofen
• ACE inhibitors (a class of blood pressure medications)
The generic names of these medications end in “pril” such as lisinopril. ACE inhibitors can cause swelling at any time during the course of therapy, even after years of being on the medication.
• Hereditary angioedema (swelling)
Hereditary angioedema (HAE) is a rare genetic disorder in which patients have a defect in the gene that controls a regulatory blood protein called C1 Inhibitor. When C1 Inhibitor does not function properly, fluids can shift out of the blood and into tissues to cause swelling. Antihistamines, corticosteroids and epinephrine will not be effective in treating swelling in patients with HAE, however targeted treatments are available once your diagnosis is established. Over 50% of patients with HAE will have their first swelling episode prior to age 12.
• Acquired angioedema
Acquired angioedema (swelling) is an acquired form of C1 inhibitor deficiency that can occur in certain diseases. This is not hereditary or passed to your children.
Angioedema without Urticaria
|
Spontaneous
|
Medication induced
|
Underlying disease
|
|
Unclear cause
Autoimmune
|
Aspirin/NSAID induced
ACE inhibitor induced angioedema
|
Hereditary angioedema (HAE)
Acquired angioedema
|
Hives and Angioedema Treatment & Management
The goals of treatment are to:
• Provide relief of itching
• Make hives more tolerable
• Provide complete resolution of your hives
Medications will help your itching and reduce hives. Medications will not “cure” hives but can help to completely resolve them. Antihistamines are the best initial medication to treat your hives. Sometimes, a combination of several antihistamines or an increased dose of one antihistamine may be recommended.
Older antihistamines such as Benadryl (sedating antihistamines) may cause you to get sleepy, cause dryness and only last for several hours. Newer non-sedating antihistamines are less likely to make you sleepy. They have fewer side effects and last much longer. Non-sedating antihistamines (shown below) are often the first medication doctors will prescribe for your hives. High dosages, up to 4 times the recommended dose, are often well tolerated and can help control your itching. This will also help to prevent the use of other medications that may have more side effects.
About 50% of chronic spontaneous urticaria (hives over 6 weeks with no identifiable cause) will respond to antihistamine as discussed above. For those who do not improve on antihistamines, 65% respond to omalizumab (Ref 2). Omalizumab is an FDA approved treatment of chronic urticaria. This medication is injected under the skin once a month. Corticosteroids, such as prednisone or prednisolone may help hives. These are not an ideal treatment for long-term use but may have a role to relieve severe symptoms for a few days.
Your doctor will outline a treatment plan that allows you to increase treatment during an outbreak of hives or swelling and reduce medications when the hives or angioedema are not as bothersome.
Chronic hives can last for many years but will often go away. Hives will resolve in half of patients within 1-2 years and 80-90% of patients will improve within 5 years. Even if a patient’s hives improve, it is not unusual to see the hives recur months to years later.
Antihistamines commonly used to treat urticaria:
|
Sedating antihistamines
|
Non-sedating antihistamines
|
|
hydroxyzine (Atarax)
|
cetirizine (Zyrtec)
|
|
diphenhydramine (Benadryl)
|
levocetirizine (Xyzal)
|
|
|
fexofenadine (Allegra)
|
|
|
loratadine (Claritin)
|
|
|
desloratadine (Clarinex)
|
References
1. Bernstein JA, Lang DM, Khan DA et al. The diagnosis and management of acute and chronic urticaria: 2014 update. J Allergy Clin Immunol. 2014;133:1270-7
2. Kaplan AP. Therapy of chronic urticaria: a simple, modern approach. Ann Allergy Asthma Immunol. 2014;112:419-25
3. Zuraw BL, Bernstein JA, Lang DM et al. A focused parameter update: hereditary angioedema, acquired C1 inhibitor deficiency, and angiotensin-converting enzyme inhibitor-associated angioedema. J Allergy Clin Immunol. 2013;131:1491-3
Find out more about skin allergies.
Test your knowledge and see how much you know about hives.
The AAAAI's Find an Allergist / Immunologist service is a trusted resource to help you find a specialist close to home.
6/2/2024