Oral Allergy Syndrome (OAS)
 If you suffer from hay fever (allergic rhinitis) caused by pollen, your mouth or throat may become itchy after eating an apple or celery. This happens in up to 50 to 75% of adults allergic to birch tree pollen. This reaction occurs because the proteins found in some fruits and vegetables are very similar to those found in pollen. These proteins can confuse the immune system and cause an allergic reaction or make existing symptoms worse, which is referred to as cross-reactivity. In the case of pollen and foods, the result of cross-reactivity is called Oral Allergy Syndrome (OAS) also known as Pollen Food Allergy Syndrome (PFAS).
If you suffer from hay fever (allergic rhinitis) caused by pollen, your mouth or throat may become itchy after eating an apple or celery. This happens in up to 50 to 75% of adults allergic to birch tree pollen. This reaction occurs because the proteins found in some fruits and vegetables are very similar to those found in pollen. These proteins can confuse the immune system and cause an allergic reaction or make existing symptoms worse, which is referred to as cross-reactivity. In the case of pollen and foods, the result of cross-reactivity is called Oral Allergy Syndrome (OAS) also known as Pollen Food Allergy Syndrome (PFAS).
OAS is a form of a contact allergic reaction that occurs upon contact of the mouth and throat with raw fruits or vegetables. The most frequent symptoms of OAS include itchiness or swelling of the mouth, face, lip, tongue and throat. Symptoms usually appear immediately after eating raw fruits or vegetables, although in rare cases, the reaction can occur more than an hour later. OAS is generally considered to be a mild form of food allergy. Rarely, OAS can cause severe throat swelling leading to difficulty swallowing or breathing. In a person who is highly allergic, a systemic reaction, called anaphylaxis (an-a-fi-LAK-sis), may be caused by a pollen cross-reactive raw fruit or vegetable, but this is very uncommon. OAS can occur at any time of the year.
Although there is no definitive test for OAS, affected individuals often have a positive allergy skin test or blood test for specific pollen, along with a history of symptoms after ingestion of the suspected foods.
Different Reactions Based on Different Allergies
Some people report symptoms with only one food and others with many different fruits and vegetables. Some people report that only certain varieties of the fruit cause symptoms, for example specific apple varieties.
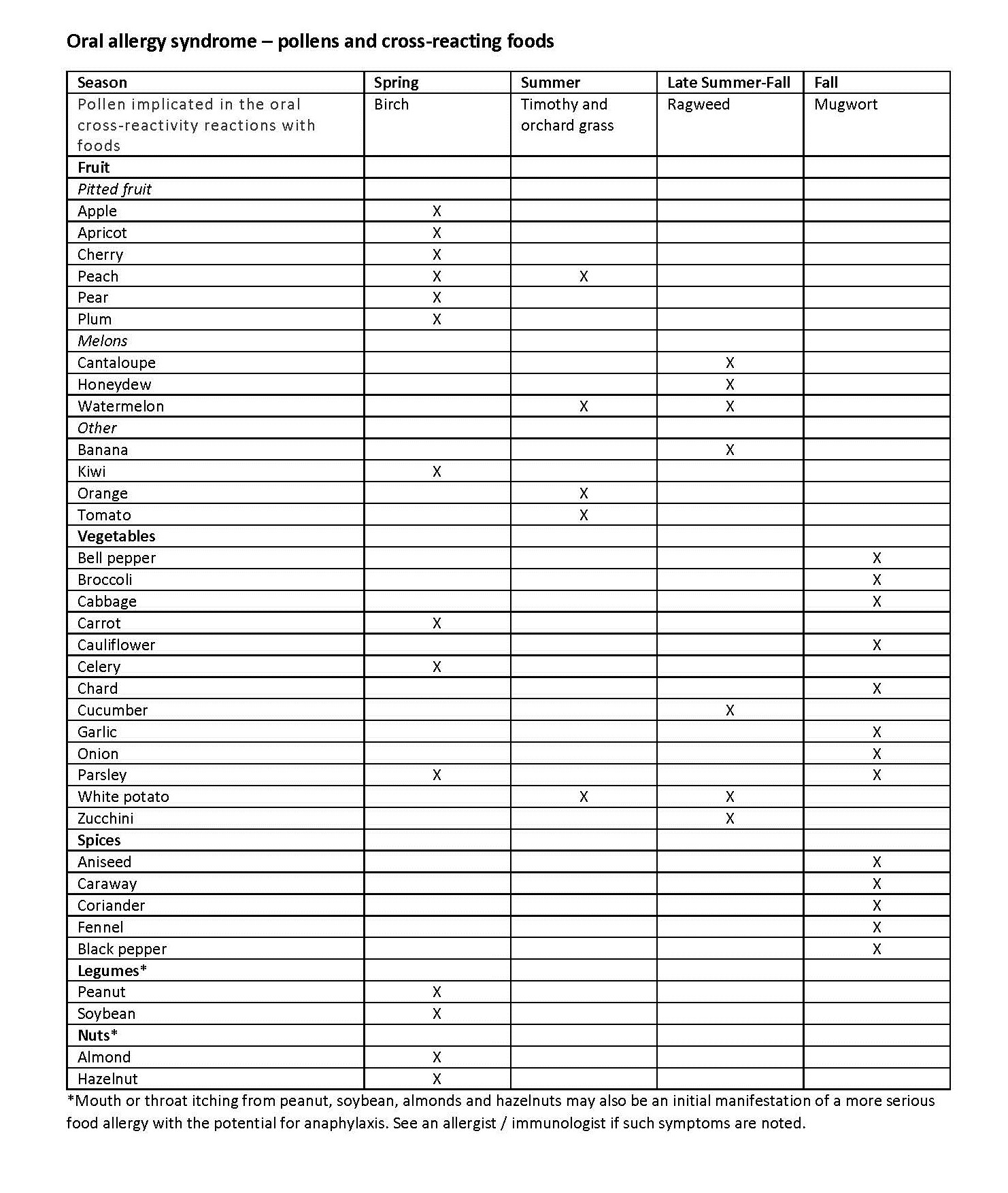
In the case of OAS, individuals react to different foods based on what type of seasonal allergies they are affected by. For instance, if you are allergic to birch tree pollen, a primary airborne allergen responsible for symptoms in the springtime, you may have reactions triggered by pitted fruit or carrot. Even peanuts, almond, and hazelnut may cause mouth itching in those with birch pollen allergy. If mouth itching is noted with nuts, you should see an allergist /immunologist because mild mouth symptoms may signal a more serious allergic reaction to nuts. People with allergies to grasses may have a reaction to peaches, celery, tomatoes, melons (cantaloupe, watermelon and honeydew) and oranges. Those with reactions to ragweed might have symptoms when eating foods such as banana, cucumber, melon, and zucchini. This convenient table lists the possible pollen and plant food cross-reactivities.
Managing Your Symptoms
If you have symptoms of OAS, avoid eating these raw foods, especially during allergy season because in many patients, OAS worsens during the pollen season of the pollen in question. One way to reduce cross-reactions with food is to bake or microwave the food because high temperatures break down the proteins responsible for OAS. Eating canned food may also limit the reaction. And, peeling the food before eating may be helpful, as the offending protein is often concentrated in the skin.
Some studies have shown that treatment with allergy shots can improve the symptoms of OAS.
You should talk to your physician if:
• Your OAS symptoms are causing significant throat discomfort;
• Your OAS symptoms are getting progressively worse;
• Your OAS symptoms are caused by cooked fruits and vegetables;
• Your OAS symptoms are caused by nuts;
• You develop systemic reactions after eating raw fruits or vegetables such as hives, vomiting or difficulty breathing.
Please note that this list is not exhaustive.
Click here for a PDF version of the chart.
Find out more about allergic rhinitis or hay fever.
The AAAAI's Find an Allergist / Immunologist service is a trusted resource to help you find a specialist close to home.
1/10/2024