Billing and Reimbursement
 Billing and Reimbursement
Billing and Reimbursement
The relationship between telemedicine reimbursement and access to care is evolving.
Telemedicine has the potential to improve access to care and reduce healthcare expenditures. Examples:
• In the emergency setting where specialists may not be on site, virtual consultations can limit the need for transportation of patients to other facilities for care. Estimates predict that teleconsults can obviate the need for up to 850,000 transfers and save $537 million per year.
• Specific to allergy, a pilot study of 50 patients utilizing telemedicine to evaluate patients for penicillin allergy demonstrated high patient satisfaction and potential savings of over $30,000 due to increased access to specialty allergy care and improved antibiotic stewardship.
There are ongoing efforts from multiple patient and physician advocacy groups for permanent laws providing parity of coverage and reimbursement for telemedicine services.
• Coverage parity = both in-person and telemedicine services are covered for the same indication
• Payment parity = reimbursement for telemedicine services approximates that of the equivalent in-person E/M service.
o As of September 2023, twenty-four states have an explicit requirement for payment parity within the law.
Parity increases adoption of telemedicine.
• Almost 90% of both users and non-users (of telemedicine) said they would use telehealth if they were to be reimbursed.
• A 77.5% increase in telehealth adoption was noted after implementation of parity in Michigan.
References:
http://www.amdtelemedicine.com/telemedicine-resources/documents/ATATelemedicineResearchPaper_impact-on-healthcare-cost-and-quality_April2013.pdf
Mary L. Staicu, Anne Marie Holly, Kelly M. Conn, Allison Ramsey. The Use of Telemedicine for Penicillin Allergy Skin Testing. The Journal of Allergy and Clinical Immunology: In Practice, Volume 6, Issue 6, 2018, Pages 2033-2040
Telehealth Index: 2019 Physician survey. American Well 2019. https://static.americanwell.com/app/uploads/2019/04/American-Well-Telehealth-Index-2019-Physician-Survey.pdf Accessed May 15, 2020.
https://www.ajmc.com/newsroom/lack-of-reimbursement-barrier-to-telehealth-adoption
https://www.forbes.com/sites/quora/2018/07/31/what-are-the-latest-trends-in-telemedicine-in-2018/#7f61f19a6b9e
https://www.cchpca.org/policy-trends/
Variability In Reimbursement Rules Among States Contributes To Confusion
No two insurers or states are alike in how they define or cover telehealth services.
• Currently, 43 states, Washington, DC, and the U.S. Virgin Islands have laws that govern private payer telehealth reimbursement policies.
• All 50 states and Washington, DC, provide reimbursement for some form of live video in Medicaid fee-for service, with fewer states covering store-and-forward or remote physiologic monitoring.
Know if your site qualifies for billing an originating site fee, facility fee, or transmission fee. Currently, 17 states and DC have a specific list of sites that can serve as the originating site for a telehealth encounter. 35 states will reimburse either a transmission, facility fee, or both. Be familiar with the rules if the referring physician and the consulting physician are at the telemedicine visit at the same time. For example, the consulting physician would bill for the visit and the referring physician would bill an originating site or facility/transmission fee if the visit was conducted while the patient was located at the referring physician’s office.
Interactive 50 state map of telemedicine reimbursement policies
https://jamanetwork.com/SsoTokenHandler.ashx?returnUrl=https%3a%2f%2fedhub.ama-assn.org%2fsteps-forward%2fmodule%2f2702689&instSigninUrl=&referralUrlKey=
CMS Has Made Sweeping Changes In Telemedicine Reimbursement, Designed To Improve Access To Care
CMS has historically placed strict limits on criteria for telemedicine reimbursement:
• Rural location of patient
• Originating site must be a health center
• Service must be synchronous live video
https://data.hrsa.gov/tools/medicare/telehealth
However, these strict limits on telehealth services may have contributed to thwarting innovation and increased adoption of new technologies, thereby limiting access to care. Therefore, CMS has pivoted to enhanced coverage of telemedicine over the last few years.
Changes in 2019:
• Brief communication technology-based service (e.g., virtual check-in, HCPCS code G2012)
• Remote evaluation of pre-recorded patient information (HCPCS code G2010)
• Interprofessional internet consultation (CPT codes 99452, 99451, 99446, 99447, 99448, and 99449)
Changes in 2020:
• Expanded access for Medicare Advantage enrollees
• Part of government funded “basic benefits” instead of supplemental services
• Available to enrollees in both urban and rural areas
• Removed requirement to go to a health care facility as the originating site of service, instead, patient can receive telemedicine services from home
For calendar year 2021, CMS finalized the addition of the following services to the Medicare telehealth list, which remain covered after the end of the PHE on May 11, 2023:
• Group psychotherapy
• Psychological and neuropsychological testing
• Lower-level domiciliary, rest home, or custodial care services, established patients
• Lower-level home visits, established patients
• Cognitive assessment and care planning services
• Visit complexity inherent to certain office/outpatient evaluation and management (E/M)
• Prolonged services
https://s3.amazonaws.com/public-inspection.federalregister.gov/2018-24170.pdf
https://www.cchpca.org/sites/default/files/2018-11/FINAL%20PFS%20CY%202019%20COMBINED_0.pdf
https://www.cchpca.org/sites/default/files/2018-11/Finalized%20PFS%202019%20Infographic%20Final%20V.%204.pdf
https://www.cms.gov/newsroom/press-releases/cms-proposes-modernize-medicare-advantage-expand-telehealth-access-patients
https://www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year-1
Medicaid Has Generally Had Broader Coverage For Telemedicine Services Than Medicare, But It Varies From State To State
The current state of Medicaid reimbursement:
• Fifty states and Washington DC provide reimbursement for some form of live video in Medicaid fee-for-service
• Thirty-three state Medicaid programs reimburse for store and forward delivered services, and an additional five states have laws requiring such reimbursement in the absence of an associated Medicaid policy (through communication technology-based service [CTBS]). States that only provide reimbursement for teleradiology were not counted in this number.
• Thirty-seven states reimburse for remote patient monitoring (RPM).
• Forty-three states and Washington DC reimburse for audio-ony telephone visits in some capacity, which has doubled since Spring 2021.
• Thirty-five states provide a transmission and/or facility fee
https://www.cchpca.org/policy-trends/
Commercial Insurers Are Focused On Cost-Savings And Operational Efficiency
Forty-three states, Washington DC, and Virgin Islands have laws that govern private payer reimbursement of telehealth. Most jurisdictions only require parity in covered services, not reimbursement amount, and depending on how the law is written, may provide payers with the ability to limit the amount of that coverage. 24 states have laws mandating payment parity for at least one specialty. Not all laws mandate reimbursement.
https://mhealthintelligence.com/news/study-states-private-payer-laws-are-harming-telehealth-growth
https://www.cchpca.org/policy-trends/
Self-Payment Remains An Option For Those Patients Without Insurance Coverage For Telemedicine Services
Although not ideal, many patients would prefer to pay a convenience fee to access non-covered telemedicine services. Costs vary significantly but tend to be lower than the charges for an in-person evaluation.
In 2020, COVID-19 Ushered in A Dramatic Expansion of Telemedicine
In 2020, governments and payers rapidly expanded telemedicine coverage and payment in an effort to ensure public access to healthcare in the midst of an infectious pandemic. As part of the expansion of telehealth services during the COVID-19 public health emergency (PHE), a number of remote services which were previously non-covered by payers gained temporary coverage. In addition, reimbursing for telemedicine visits at the same rate as in-person visits has been instrumental in encouraging increased telemedicine adoption among providers during the PHE.
For the most part, states continue to keep their temporary telehealth COVID-19 emergency policies siloed from their permanent telehealth policies. This gives jurisdictions flexibility to revert to their permanent policies once the PHE comes to an end. However, extensive lobbying is occurring to make at least some of the COVID-19-associated telehealth reimbursement expansion permanent.
As of 2023, the following telehealth expansions have been made permanent by CMS. However, they typically will not impact allergy/immunology practices.
• Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) can serve as a distant site provider for behavioral/mental telehealth services
• Medicare patients can receive telehealth services for behavioral/mental health care in their home
• There are no geographic restrictions for originating site for behavioral/mental telehealth services
• Behavioral/mental telehealth services can be delivered using audio-only communication platforms
• Rural Emergency Hospitals (REHs) are eligible originating sites for telehealth
Although the COVID PHE has officially ended, the following temporary telehealth expansions will remain in place through 2024.
• FQHCs and RHCs can serve as a distant site provider for non-behavioral/mental telehealth services
• Medicare patients can receive telehealth services in their home
• There are no geographic restrictions for originating site for non-behavioral/mental telehealth services
• Some non-behavioral/mental telehealth services can be delivered using audio-only communication platforms
• An in-person visit within six months of an initial behavioral/mental telehealth service, and annually thereafter, is not required
• Telehealth services can be provided by all eligible Medicare providers
https://telehealth.hhs.gov/providers/telehealth-policy/policy-changes-after-the-covid-19-public-health-emergency
For an updated list of state-specific actions related to the expansion of telehealth during the COVID-19 pandemic, see the following link for the Center for Connected Health Policy:
https://www.cchpca.org/covid-19-related-state-actions
A list of some updated commercial payer-specific telehealth policies is available here:
Aetna:
https://apps.availity.com/web/core/vault/vault/v1/files/336384/Kad1BQ9kR/9c41ef6d-f60d-42f4-a692-6372ce0b7230?spaceId=73162546201441548441629200000321
Blue Cross Blue Shield:
Example billing guidance from Blue Cross Blue Shield Alabama: https://providers.bcbsal.org/portal/documents/10226/3494887/Telehealth+Billing+Guide+Post-PHE.pdf/1c8040a8-090f-11f1-b9af-0e267b645385?t=1683572910617
Telehealth coverage and cost-sharing amounts (deductibles, copayments, etc.) can vary among Blue Cross plans, including the Blue Cross and Blue Shield Federal Employee Program® (BCBS FEP®). Always check eligibility and benefits through ProviderAccess or your practice management system to confirm benefits and cost-sharing details.
Cigna: https://static.cigna.com/assets/chcp/secure/pdf/resourceLibrary/clinReimPolsModifiers/R31_Virtual_Care.pdf
United Healthcare:
https://www.uhcprovider.com/content/dam/provider/docs/public/policies/comm-reimbursement/COMM-Telehealth-and-Telemedicine-Policy.pdf
Codes
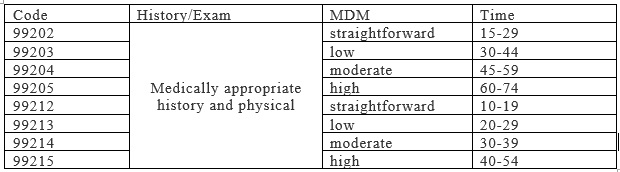
In most cases, coding for telemedicine services is done using the corresponding codes for an in-person E/M visit, but with specific modifier(s) and place of service designation to clearly identify the service as telehealth.
Code: Telemedicine coding can be based on either time or medical decision-making. As of 2021, time-based coding includes the total time spent on the encounter on the day of service, rather than only face-to-face time.
https://www.aapc.com/evaluation-management/em-codes-changes-2021.aspx
Modifier: For both private payers and CMS, the -95 modifier (synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system) should be appended to E/M codes 99202-99215. (Medicare used to require modifier GT for synchronous visits and GQ for asynchronous visits, but this was eliminated as of January 2018.)
Place of Service: Historically, the place of service has been designated as “02” on the bill to signify a telemedicine service. However, this changed for most payers in 2020 when PHE-related telehealth expansion ushered in payment parity for many telehealth services. Updated guidance for Medicare and most commercial payers was that for the duration of the COVID-19 PHE, telemedicine services should be billed using the place of service that would have been used if the service was provided in person, along with modifier -95. For outpatient allergy practices, this was place of service “11.” Doing so ensured that the claim was eligible to be paid at parity with non-facility face-to-face rates for Medicare and most commercial payers.
However, in 2022, CMS updated the list of place of service codes, adding place of service “10” to designate telehealth services provided when the patient is in the home setting. After December 31, 2023, the guidance is for place of service “02” to be used if the location of the patient at the time of the visit is outside of their home, and for place of service “10” to be used if the patient is at home during the visit. While a number of private payors have adopted similar guidance, they are not required to do so and may have their own guidance regarding how to list place of service for telemedicine. Due to this variability, it is best to check with each individual payor to determine how best to code telehealth visits, and to understand when COVID-19 specific billing and coding guidelines will expire.
Bajowala SS, Milosch J, Bansal C. Telemedicine Pays: Billing and Coding Update. Curr Allergy Asthma Rep. 2020;20(10):60. Published 2020 Jul 27. doi:10.1007/s11882-020-00956-y
https://www.cms.gov/medicare/coding-billing/place-of-service-codes/code-sets
https://www.cms.gov/files/document/mln901705-telehealth-services.pdf
CMS has provided the following pamphlet to provide coding guidance for telehealth providers:
https://www.cms.gov/files/document/telehealth-toolkit-providers.pdf
Examples of Telemedicine Coding (after December 31, 2023)
Online synchronous video visit with an established patient (who is at home) to evaluate a new onset pruritic rash. Diagnosed as atopic dermatitis and prescribed emollients and triamcinolone 0.1% ointment. 20 minute visit.
Option 1 (Private Insurance):
CPT code: 99213
Modifier: 95 (may be optional)
Place of service: 10 (required)
Option 2 (Medicare):
CPT: 99213
Modifier: 95 (optional as POS signifies telehealth)
Place of service: 10
After December 31, 2024: For non-behavioral or mental telehealth, there may be originating site requirements and geographic location restrictions for Medicare patients.
If this patient was not at home, but rather at the primary care physician’s office for a facilitated telehealth visit, place of service would be changed to 11 for the originating site and 02 for the distant site, and the following codes might also be billed:
Originating site (physical location of patient) also bills facility fee: CPT Q3014 (optional)
Both originating site and distant site also bill transmission fee: CPT T1014 (if eligible)
Online synchronous video visit with a new patient (who is at home) with multiple food allergies who wishes to obtain a second opinion about dietary management and review emergency action plan. 35 minute visit.
Option 1 (Private Insurance):
CPT: 99203
Modifier: 95 (may be optional)
Place of service: 10 (required)
Option 2 (Medicare):
CPT: 99203
Modifier: 95 (optional as POS signifies telehealth)
Place of service: 02 (required)
After December 31, 2024: For non-behavioral or mental telehealth, there may be originating site requirements and geographic location restrictions for Medicare patients.
If this patient was not at home, but rather at the primary care physician’s office for a facilitated telehealth visit, place of service would be changed to 11 for the originating site and 02 for the distant site, and the following codes might also be billed:
Originating site (physical location of patient) also bills facility fee: CPT Q3014 (optional)
Both originating site and distant site also bill transmission fee: CPT T1014 (if eligible)
These links are for research only. They are not endorsed by the American Academy of Allergy, Asthma & Immunology (AAAAI).
12/7/2023